Jeffrey Robinson, Residency Director for Emergency Radiology at HMC
11/29/2024 Several Issues
As we are now an enterprise-wide Emergency Radiology section, please accept calls from Montlake or Northwest if they call for assistance. If you cannot resole the issue, transfer to attending. Do NOT have them call someone else.
Make sure you sign out with your attending before leaving. We have had a couple of instances of ‘disappearing resident’, which is not good form.
Contrast extravasation guidelines have been updated and can be found here
Regarding coronary CTA: if you report a coronary CT or triple rule-out, please secure message the attending, so we know it’s there- we need to finalize promptly so the patient can be discharged, if appropriate
10/25/2024 Day Rotation Start Time
You are expected to be on time. Start time is 8:00 AM when there is no morning lecture, and 8:30 on days that there is morning lecture. If there is a lecture, you should attend on site at HMC (ie, in NCR).
9/3/2024 Educational Videos
UW has changed streaming applications, and all the videos have been migrated to the new syste,. However, I need to re-link the videos with the website, so be patient.
6/29/2024 Vessel Wall Imaging
In conjunction with the beginning of VWI for acute stroke in the HCMED, we have posted an introductory powerpoint by Dr. Hartman on the website under the “Tutorials/Basic Material” link. Check it out…
12/15/2023 IMPORTANT: Updated Ultrasound callback rules
Starting 12/15, US exams requested from the HMC ED will follow limited indications during the hours 7pm to 7 am. We used to allow sonographer call back for any ED exams until 10 pm. Unfortunately, staffing shortages require fewer call backs for our sonographers. EM has agreed to this reduction.
10/12/2023 Outside Reports in Visage
Visage files the outside reports on transfer patients in the “paperwork” series at the end of the exam, behind the dose report screen shot.
10/6/2023 Basic Housekeeping
Ladies and gentlemen: at the end of your day, please clean up your work area. Papers go in the shredder, cups and uneaten food go in the recycling, etc. The reading room has been getting a little grotty lately.
5/10/2023 Restating of Existing Spine Policy on Transfer Patients
Spine reformats of outside studies are RARELY needed. If you receive such a request, review the outside exam MPR’s, and unless they are uninterpretable, you may use those images to clear the spine.
5/5/2023 Clarification on HED responsibilities
HED duty hours are now 8AM to 5PM (rather than 6PM as it has been previoously). Morning conference continues to take precedence over 8AM start time.
Note: R2 residents are not to issue preliminary reports on neuro exams (ie, head CT) or non-ED exams (formerly known as ‘call cases’).
10/26/2022 Updated Contrast Reaction Algorithms
Dr. Wang and the Contrast Committee have updated the treatment algorithms for contrast reactions to make them more relevant to what we do in our department. The link has been updated, so check it out here
https://sites.uw.edu/eradsite/jeff8rob/trauma-radiology-reference-resource/5-general-and-miscellaneous/treatments-for-acute-reactions-to-iodinated-contrast/
5/10/2022 Iodinated Contrast Shortage
Current (as of the faculty meeting today) procedures are taped on the wall in the ER reading room.
The following e-mail was sent out to the entire medical staff on May 6:
Sent on behalf of UW Radiology LeadershipDear Colleagues:We wanted to provide a status update regarding iodinated contrast shortages due to a factory closure in Shanghai, China that has affected GE Healthcare’s production of Omnipaque and Visipaque.We are actively tracking our inventory across each site and will work to share resources between UWMC campuses, HMC, and FHCC (SCCA).We have performed initial projections. Based on the contrast we have in hand, we will run out of iodinated contrast across the enterprise by end of business day on Monday, May 9th. GE Healthcare has promised a large shipment of contrast medium to be delivered that same day. If this arrives as promised, we will have contrast across the enterprise for about 10 business days. [ed note: the shipment arrived, and we are good until perhaps the end of June]While we would like to be optimistic, given challenges and irregularities with shipping and potential for overpromising and underdelivering, we are pursuing a strategy that accounts for contrast in hand only.As such, we would like to declare that we are indeed in a crisis situation, and that, given the potential that contrast-based imaging can facilitate life-saving information and intervention, we should engage with disaster command center in the scenario that we imminently run out of iodinated contrast.Our leadership team met this AM, and we have created three tiers of imaging priority:Tier 1: Emergent and urgent angiography-based procedures (cardiology and angiography), and Acute care/emergency imagingTier 2: Oncology imagingTier 3: All other imagingWe are also actively creating Section-based approaches to convert contrast-based imaging to non-contrast imaging or alternative modality imaging (e.g., ultrasound or MRI). We plan to implement those changes beginning today.Our specific asks:
- Assist with initial discussions with disaster command
- Assist with communication to providers that we will be changing some examinations to non-contrast to conserve this resource. Because of the volume of changes, we will not have time to call each provider. We will send a courtesy SecureChat message to the ordering provider. (We acknowledge that some providers do not use SecureChat; however, we cannot have multiple processes)
- We would like to send out a communication from your leadership group announcing these mitigation strategies.
As it relates to our most critical patients in Tier 1, Jonathan Medverd will be working with Susan Stern to develop an optimized imaging strategy to decrease contrast use while also maintaining high quality patient care and imaging. I will also ask Evan Johnson to assist with communication and resource management across IR and non-IR angiography procedures.Thank you all for your support as we manage this crisis together.Sincerely,
Habib Rahbar, MD; VC of Clinical Operations and Chief of Service, UWMCJonathan Medverd, MD; Chief of Service, HMCCarolyn Wang, MD; Chief of Service, FHCCMichael Doherty, MD; Site Director, UWMC-NWSteven Chung, MD; Site Director, UWMC-ESC
12/20/2022 COVID Reminder
ED Radiologists should maintain wearing their masks as long as they are not actively drinking. They can take one side of the mask down while on the phone, then fully cover their nose and mouth when done.
10/12/2021 No More Spine Reformats of Outside Exams
9/9/2021 Reporting Trauma Series
With the new systems in place, we will no longer be associating chest and pelvis radiograph reports for trauma series. Please report these exams separately, as 1V Chest and 1V Pelvis.
8/11/2021 Misc reminders
A few things have come up recently which are not new but bear re-enforcing:
- Spine reformats on outside CT scans RARELY need to be done at Harborview. The sagittal images from the outside are usually sufficient. Our standard is that if one of the imaging planes is 3mm slice thickness or thinner, then the exam is considered adequate. If the outside images are technically inadequate, rescan the patient here.
- Please identify yourself as a physician when answering the phone. Callers frequently get the wrong number and don’t know if they are talking to a clerk, a nurse or a doctor. It’s not a power thing, it’s a disclosure thing.
- While we are all adults and can manage our own time, we need you to check in and out with the attending. It’s not a permission thing, but we are responsible for knowing where the residents are, who’s not. This is particularly relevant in the morning when night residents are leaving.
6/30/2021 Review at the scanner
With the regression of the COVID pandemic, we will resume our former workflow of reviewing Pan Scan and Stroke Code exams at the scanner starting July 1.
3/21/2021 MRI Call Prep
Charlie Davis and JJ Weaver have compiled a selection of MR exams that represent what you may see on call. They can be found in the Tutorials section, replacing the Protocoling and Worklist creation tutorials that will no longer be relevant after D1 next week.
12/10/2020 Northwest Hospital Coverage
As you know, HMC ED is transitioning to covering Northwest Hospital after hours. Currently there is resident coverage from UW until 11:30 PM Monday through Friday. After that, ED exams are either covered by the UW overnight attending or go to VRad (until we are fully staffed at night). Inpatient exams are covered upon request by the UW Overnight Attending, or are read in the morning. There MAY be occasions in which a preliminary resident report is requested overnight on an inpatient. Please dictate if requested.”
9/24/2020 ERad Guide updates
Further updates to the resident guide concerning professionalism, inpatient studies and calling IT Helpdesk at night.
9/9/2020 Professionalism
The section in both the Day Guide and the After-Hours Residents’ Guide has been edited. Please read it over, especially with reference to checking in/out with the attending.
7/1/2020 Edit to Outside Read macro
Note that there is a new line on the template for transfer patient overreads. Billing requires us to note when MIPs are done for a CTA, so there is a new line to delete for non-CTA overreads. I thought it would be easier to make it a deletion than to ask people to remember to put such a statement in whenever an outside CTA is done.
4/23/2020 New Pulsara acute stroke algorithm
Please see the updated Acute Stroke Protocol Imaging page to find the revised algorithm for acute strokes. We are now using Pulsara to communicate with the stroke team. You may download the Pulsara app to your mobile device or use the iPad mounted in the ERad reading area.
4/6/2020 SPECIAL: COVID Edition
Here are a few adjustments we have made in the HMC ERad to deal with social distancing and coronavirus protection:
2/25/2020 Sheath Introducer for CT injections
The ban on using the side arm of a catheter introducer sheath (aka ‘Cordis’) has been lifted. Effective immediately, if a critically ill patient has no other venous access, it is OK to use the sheath side arm for CT contrast injections. Link to updated policy here
12/2/2019 New and improved core videos
We have updated the ERad video collection in two ways. The 2019 course is available in its entirety here. Also, we have updated the core video collection for the daytime rotation. The link location is the same, but the segments are now identified with specific teaching sessions, and there are both basic and advanced segments. The basic segments are expected viewing for the HED rotation; the other segments are optional, but useful for higher level residents.
8/28/2019 Using dictation Macros
Emergency Radiology makes extensive use of report macros. This improves report accuracy and completeness, as well as allowing for data mining. Use the default exam macro that comes up with your exams unless it is either the incorrect macro, or there is some compelling reason to do otherwise.
8/17/2019 Trauma Series Reminder
Remember that for full trauma activations, you are expected to accompany the tech into the trauma bay and provide a ‘wet’ reading off the low-res monitor embedded in the portable unit. The Schedulers and/or techs will notify you of a full trauma activation (as opposed to a modified trauma activation, which is less critical).
10/19/2018 Radiation in Pregnancy
Dr. Knight has created a new concise reference for providers (that’s us too) on radiation risks in pregnancy. It is designed to give the clinicians the information they need to talk to patients, but is good reading for radiologists, too. The link is the same on the front page of the website, but it links to a PDF document which you can print out or forward.
7/12/2018 VA Ultrasound update
MOU for transfers for testicular US is official. VA is still working on US call.
7/9/2018 VA Ultrasound update
Actually an update as of June, but here is the text of an e0mail from Suresh Maximin from the VA. I will update the status of on-call VA US as I hear about it:
I just spoke to the ED chief here. she has been trying to get UW ED to sign off on testicular US transfers, and this is now the final barrier. She is hoping to have an answer shortly. She resent a request today to get their sign off. She did clarify the prescription issue, so that should not be a barrier for a VA patient.
Oncall attendings for the VA are in Amion, but if for some reason it’s not updated, which has happened, the UW resident gets a call from me. The residents also are aware that the off hour techs here and the VA operator will know who is covering
there has not been a sonographer on call here bc their pay had been abysmally low. I stood over the CFO’s shoulder last week watching him finally sign off on a big salary increase for them. as soon as that is finalized with HR, we will have US on call, so all of this should theoretically go away.
in the meantime, until the UW signs off on the transfer MOU for testicular cases, the ED chief here is hoping that we can have a resident come over, but she is aware that there is a high likelihood that they may not be available because of other duties, so she is pushing hard to get UW signoff on transfers ASAP.
Thanks very much
Suresh
6/27/2018
The new ED portable X-ray units have embedded low-res screens, which requires a change in our workflow for trauma series. The ED docs are seeing these images before we do, and we risk becoming irrelevant. Therefore, when a trauma code is called, the scheduler will notify the radiologist of the impending trauma series. The rad accepting the case will accompany the tech over to the trauma bay and give whatever qualified interpretation we can from the small screen as the images are taken. Feel free to hedge and let them know that you will come back across the hall if the workstation interpretation is different. A link to the formal workflow is here.
5/7/2018 Clarification regarding Pediatric CT
If there is a question about a pediatric CT, your first call is to the ERad attending. It is not necessary (or appropriate) to call the Children’s Hospital on-call services unless directed to by the HMC ERad attending.
3/27/2018 New Website Content
I added a new link to a page containing images of power-injector compatible ports. These are the ones I could find. If you know of another brand, send it to me and I’ll add it to the page.
2/16/2018 Updated Code Stroke protocol
The code stroke imaging algorithm is being updated to do MRI for basilar artery thrombosis. The updated workflow can be found here.
2/7/2018 Two updates
1. Recordings of this last summer’s ERad 2017 course are available here:
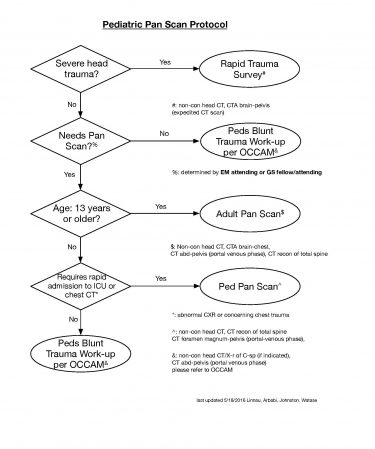
12/12/2017 Updated Pediatric Trauma Imaging Protocols
Revisions to the pediatric imaging algoriothm were recently approved at Trauma Council. The goal was to eliminate the different age cutoffs that different body part imaging protocols called for. A secondary goal was to speed the imaging of critically injured pediatric patients by doing CT rather than plain films of the spine in some occasions. The protocol will be updated in OCCAM shortly, but in the interval, you can access a flowchart here.
12/2/2017 Updated Acute Stroke Protocol Imaging Algorithm
Last week there was a multidisciplinary meeting trying to address the impression that we are overusing CTP (CT perfusion), in that it is really only useful in patients who have a large vessel occlusion (LVO, only found in a small minority of our stroke codes). So, to address this, we will be changing the order of our Stroke Code CT imaging. The new algorithm is described here
11/22/2107 Clarification on Sudden Cardiac Death CT protocol
This is a research protocol with explicit inclusion and exclusion criteria. It cannot be combined with other scan protocols. Per Dr. Gunn, these are the criteria:
Study population:
All survivors of idiopathic sudden death, including presumed idiopathic sudden cardiac death, that reach the Emergency Department and who are clinically stable to undergo CT scanning.
Inclusion Criteria:
- Patients reaching the Emergency Department within 6 hours of resuscitated idiopathic sudden death (any initial cardiac rhythm).
- Cause of the sudden death episode is not obvious to the treating ED physician (i.e., a idiopathic sudden death event) after acute initial evaluation with standard of care.
- Clinically stable to have CT performed per treating physician.
- Candidates for continued intubation and sedation during the CT scan with or without therapeutic hypothermia protocol.
Exclusion Criteria:
- Meets criteria for acute ST elevation myocardial infarction (ST elevation ≥1 contiguous lead or new or unknown duration left bundle branch block on ECG)
- Obvious cause of sudden death – Examples: witnessed trauma, drowning, suicide attempt
- Known non-revascularized coronary artery disease or coronary stent <2.5 mm.
- Known severe renal dysfunction (baseline eGFR<30 ml/hr, creatinine >1.7 mg/dl)
- Implantable defibrillator, due to metal artifact from defibrillator coil
- Known iodinated contrast allergy
- Known hospice patient or terminal disease with expected <3 months survival
10/30/2017 Outside Image Interpretation Clarifications
-
Outside imaging of the spine is adequate if one of the reconstruction planes (sagittal, axial or coronal) is 3mm or less in thickness. If no place is 3mm or less, then retros from thin slice data will be needed, If those are not available, then consult with the clinicians regarding re-imaging (plain film or repeat CT).
-
When dictating a full report due to missing outside report, delete the word “None” under “Discordant Findings”, and import the Findings and Impressions from the appropriate site macro under the “Findings/Impressions” heading.
-
Dictation macro updates:
Reasons for changes:
- Reduce variability in workflow between attending on site and overnight.
- Reduce the number of T and L-spine requests.
- Address issue of outside report arriving after dictation
Changes:
- Day and evening residents should no longer delete the “preliminary report dictated by” and “unless a comment…”. ERad attendings will add the attending final macro on all outside reports.
- Under the heading Clarifications, a statement has been added regarding the spine. If the exam does not contain spine images, then delete the statement. If it does, either select the appropriate section (if the spine is intact) or describe the fractures, (if it isn’t). If the outside report impressions (which were already dictated) clearly address the spine, delete this sentence.
- New default text under the heading Outside Report Impressions says, “Outside report not available at time of dictation.” If the report is available, replace this text with the impressions. If not, leave it in place. Now if the report arrives after the HMC dictation is done and is scanned into PACS, we have clarified that we did not see it when reporting the study out.
10/24/2017 Updated Outside Image Interpretation Macro
The macro we use for transfer patient scans is still evolving. The last improvement added a statement about spine imaging, to reduce the number of T-L spine retros we are asked to do. There will soon be a modification to that statement requiring you to choose which spine segment is being reported (Cervical, T-L, etc.) That positive action indicates that we have actually looked and evaluated the spine. Obviously, of there is not a spine on the exam being reported (like a knee or head CT), then delete the sentence alltogether.
10/12/2017 Updated policy on Transfer Patient Overreads
The formal policy that covers the new workflow dealing with exams on transfer patients is now posted here .
10/5/2017 Spines on transfer patient CTs
Clarification for spine clearance: Technically adequate outside spine CT needs to have at least one reconstruction plane at 3mm slice thickness or less. This will allow identification of the more subtle nondisplaced fractures that may not be seen with the thicker slices. Those thick slices are sufficient to identify unstable or displaced fractures.
We have also updated the outside image interpretation macro to include a default line addressing the spine. Pay attention and modify or delete the line as appropriate. This is intended to reduce the number of retro spine requests we get from the trauma services, so you can point this out to them when the requests come in.
9/25/2017 Daily resident feedback opportunity
Be sure to use the “Compare Revisions” feature of Powerscribe 360 which will show you any differences between your dictated preliminary report and the finalized report signed by the attending. It works like the ‘track changes’ feature in a word processor. Access is by highlighting an exam in your “My Reports” list, then select Tools>Compare Revisions from the top menu. In this way you can see what changes were made to your preliminary report, even minor stylistic ones which can improve your dictations.
6/27/2017: After-hours Preliminary Reports
R2 residents may not issue preliminary reports from the HMC ED for any exam that will not be overread until the next day. This particularly applies to neuro CT and inpatient CT and MRI exams.
6/27/2017: After-hours Ultrasound
There have been recent incidents in which the ultrasound tech has been called back after 10PM for an appropriate exam, but when here has been asked to do additional exams that do not meet criteria “because you’re already here.” Regardless of whether the tech is here or not, each exam after 10PM must meet the imaging criteria, because the fatigue factor for on-call techs after-hours is real. Keep in mind that they are not on a night shift like the radiologists. To reiterate: “because you’re here already” is not sufficient grounds to have the tech do an US exam after 10PM.
6/23/2017: Updated Gastrostomy Tube Check protocol
Please see updated protocol here
4/28/17: Powerscribe 360 v 3.5 new feature
When reviewing your reports in Powerscribe, select Tools> Compare Revisions (or keyboard shortcut Alt-t, Alt-i) to see differences between a finalized and preliminary report. The changes are displayed in a format similar to the “Track Changes” feature in Word. This is particularly useful to see how subtle changes in the body of a report can lend nuance to the impressions you are giving to providers.
4/28/17: Paperwork reduction act
I will no longer be placing these blog entries in a separate Word document in Lightbox. The orientation documents will still be there, but all future updates to the Harborview Emergency Radiology service will be available here. All residents are encouraged to check here before call for updates.
4/18/2017: Resident Feedback
The TR3 has a new convenient url: www.uwerad.org.
The Emergency Radiology faculty wish to share with you some information about our resident feedback processes. This is nothing new, but is a statement of what we have been doing for a long time. We post it here, and with the day rotation orientation documentation to ensure that expectations are clear from both your and our perspectives:
ERad faculty provide feedback to residents frequently. This feedback takes several forms and serves several functions.
-
Real-time feedback. When working together in the reading room, faculty overread most resident reports while the resident is still at the workstation. In this setting, the faculty may call the resident over to review a particular exam.
-
Next-day feedback. Faculty reviews many resident reports after the resident has left the service for the day. In this setting, the faculty will add addenda to reports for the resident to review when returning to the service.
-
Scheduled feedback. Verbal feedback from faculty is provided mid-rotation, and formal evaluation is performed at the conclusion of the rotation.
Faculty feedback may be for any of the following broad categories of improvement:
-
A report may have omitted an observation, or contain an interpretation that could be improved. These changes may not impact patient care at all, but provide an educational opportunity for the resident. When done in the form of an addendum, the addendum will be titled, “Attending Comment”.
-
Patient management. An omission or suboptimal interpretation may affect patient management. When this type of feedback is provided in real time, the resident can verbally inform the relevant Emergency Medicine attending of the change. If the feedback is asynchronous, a faculty addendum will be titled, “Emergency Radiology Attending Addendum”.
-
Report style. Subtle changes in report language may alter clinical decision making, beyond the bare facts of the report. Feedback on these types of issues is generally given real-time, as addenda are not really appropriate in this case.
-
Interpersonal relations. These situations rarely occur, but in the case of an issue between a resident and other providers or staff, face to face feedback is most appropriate. Formal documentation will be submitted if required by the particulars of the situation.
4/5/2017: Trauma Radiology Reference Resource (TR3)
There is a new on-line resource available in beta form here. It combines features of the Blue Book all residents were issued on their first ERad rotation with the protocol information tacked on the bulletin boards in the Emergency Radiology reading room. You are encouraged to bookmark the site for use when you are on service to have ready access to both clinical reference information and HMC-specific protocols. Please e-mail Dr. Robinson (jeff8rob@uw.edu) if you have ideas for updates or corrections.
4/1/2017: ERad resident feedback
There is a new document posted here outlining the philosophy and purpose of resident feedback in the Emergency Radiology rotations. All residents are encouraged to read it.
3/10/2017: Portable Extremity Radiographs
Occasionally techs will take portable extremity radiographs on trauma patient in the ICU. This protocol was developed after an ICU patient who was too fragile to come down for plain films was fount to have an obvious wrist fracture after several days. A link to the full protocol is here.
1/30/17: Protocoling Pan Scan Spines
Be sure to select “ERAD Full Spine Retro” when protocoling Pan Scans. Otherwise the incorrect technique gets pulled in to the report macro by Powerscribe.
1/17/2017: Evaluation of neck vessels in Pan Scans
Due to recent occurrences of BCVI in Pan Scan patients who did not meet our criteria for neck CTA, we have been requested to screen all Pan Scans for BCVI. In order to make this possible, the CTA portion of the Pan Scan is now reconstructed at 1.5mm slice thickness. We are expected to specifically review the vertebral and carotid arteries. If you find anything suspicious then ask the techs to retro out a formal neck CTA.
The Pan Scan macro reflects this increased level of scrutiny.
Additionally, while we were at it, we eliminated the sagittal obliques (candy cane views of the aorta) from the recons and added a more standard sagittal recon of the chest instead.
12/12/2016: ERad resident responsibility for inpatient exams
A reminder of the current status, one that has not changed: After hours, the emergency radiology team (residents, fellows and faculty) are the first point of contact for issues arising for inpatients as well as ED patients (and rare out patients). We are to protocol CT and MR exams on an urgent basis when requested by the techs, and review any cases that clinicians need a preliminary report on. After giving such a report, please use the preliminary report macro and dictate a summary of your communication.
11/10/2016: RV:LV ratio for CTPA
For all positive HMC CTPE scans, report RV to LV ratio:
• Use transverse (axial) CT images for measurement
• Recommended measurement technique is “maximal diameter through stack”
• Report actual ratio if possible (quantitative)
• Can use new picklist in impression:
– RV/LV ratio =>1.0: right heart strain likely
9/9/2016: Outside CT Spines.
January 2016 updated protocol. Reposted without change here.
Summary: HMC reformats no longer required for reporting of spine imaging on outside CT exams
New procedure:
- ED requests formal spine report on outside CT exam.
- Radiologist looks at images and decides if the image quality is adequate.
- If the radiologist believes the image quality is adequate, radiologist dictates report from the existing outside images.
- If radiologist believes the image quality of the spines is not adequate, then the radiologist asks the techs seek thin section axial OSH images and perform reformats, then dictates report.
Rationale:
Outside facilities have greatly improved the quality of their scans over the last several years. Most exams have satisfactory sagittal and coronal reformats. If the image quality is inadequate, the provision still exists to have our techs reformat satisfactory MPRs.

9/3/2016: Critical transfer patients will be processed with priority
Patient information will be listed on the Radiology Transfer Whiteboard as usual.
This alerts the file room to quickly obtain imaging (and reports), whether or not the patient is transferred to HMC.
If MD determines patient is to be transferred to HMC as a Critical Transfer, then the following occurs:
The Transfer Center will create an entry in the Tracking Shell, and will include the text “CRITICAL TRANSFER” on the top line of the “Reason For Visit” field.
This will identify those patients whose outside imaging should be reviewed as a priority.
The file room will call emergency radiologists at 744-3651 to notify them of the critical transfer. Information about this patient will be on the Tracking Shell, so radiologists can determine their name, ETA and other relevant information.
During normal working hours for neuroradiology, if there are imaging studies that neuroradiology normally processes, the file room will call neuroradiology (744-6143) to alert them to the critical transfer and the studies they should review.
8/10/16: Hand Hygiene
Note that when there is a patient in CT, the CT control area is defined as a patient care area. This means that you must gel in-gel out of the CT control area when you go into the control area, such as for checking for delays, stroke codes, etc. The boundary is identified by a green stripe on the floor at the entry to the CT control area.
7/19/2016: Work hours policy
All residents are expected to arrive at the beginning of their assigned shifts and to stay until the end of their assigned shifts, unless explicitly arranged with the attending who will be affected by the absence. [JR]
6/28/16: Pediatric Pan Scan
November 2014
11/25/14: ERad US studies will now be reported under the ERad attending on service, 24/7. Please check each study to ensure that the correct attending is assigned to the report by the sonographer, and correct if necessary. [JG]
11/17/14: New protocol implemented for overnight brief preliminary interpretations of inpatient Body and Chest CTs. [JG] Accordingly, the instructions for the “After Hours Resident Prelim Reports” web page has been updated. See here: [MG]
October 2014
10/20/14: The PanScan was updated on 8/27/14 to extend arterial imaging through the pelvis for patients with pelvic ring disruptions. See details on “CT Trauma PanScan” page on how to protocol and report this exam. [JG]
September 2014
9/24/14: The assigned attending for dictations after 10pm shall be Support Service, rather than the AM ERad attending. This is listed as “_Support, Service” in PS360 so it can easily be found at the top of the list of attendings. ERad attendings the following morning will check the Support Service cases in PS360, and assign all ERad cases to themselves. They should be sure to do so after the last case read by the overnight residents/fellows, and not just when they start their morning shift.
Prior to 10pm, cases will be dictated under the current ERad attending, to avoid switching back and forth between attendings. [JG]
August 2014
8/28/14: Updated the “After Hours Resident Prelim Reports” page to correct the attending assigned (_Support, Service). [JG]
8/28/14: Updated recently posted “IT-PACS-RIS Support At HMC” page. This page describes who to contact for which IT support issues. [JG]
July 2014
After consultation with neuroradiology, we decided to stop performing the routine venous phase CT of the head as part of the Trauma PanScan with CTA Neck. [MG]
March 2014
The procedure for calling in the sonographer after hours has been updated, and is available on this website. Changes include: Contacting the sonographer through the pager operator rather than directly; Obtaining permission for after hours cases that do not meet criteria through the ERad attending or Body Imaging Fellow.
Incidentaloma section added. Three tiered system for thyroid nodules added [MG]
July 2013
7/1/13: [JG]
Pan Scan: Protocol partially implemented. MG encourages faculty to use it and report back with concerns.
Sudden Cardiac Death Protocol: There is a protocol on the Siemens scanner.This protocol is only performed when MG is available. Page MG before 10pm for these studies. If he does not respond within 5 minutes, inform ED that he is not available to perform this study, and consider other imaging options.
MARCH 2013
3/4/13: A number of trauma protocols, including their imaging components, have been updated over the past few months, and are continuing to be updated. These are posted on OCCAM, and links to these new protocols are being updated on the ERad web site as well. Some of these are summarized below. [JG]
Rapid Trauma Series. No longer has a decision to make after the noncontrast HCT. Once the study is ordered, the entire study is performed including the contrast enhanced CT of the neck, chest, abdomen and pelvis.
Indications for spine imaging have been updated.
3/4/13: Outside studies. These can be dictated and merged onto PACS before the patient arrives. The Transfer Center can generate an MRN 24/7. The only glitch is that the ED cannot currently order an outside report interpretation with CPOE before the patient arrives, and this order needs to be submitted via paper request. [JG]
3/12/2013: Rapid Trauma Survey document updated. It is available here. [MG]
SEPTEMBER 2012
9/21/12: Clarification about when to obtain a CTA head vs CTA neck is provided here. [JG]
AUGUST 2012
8/31/2012: Trauma series exam codes (Trauma Series 2 View, and Trauma Series 3 View) have arrived!! [MG]
8/22/2012. New protocols for the initial evaluation of closed head injury in adults and children were approved at Trauma Council. They are available on OCCAM, a new repository for HMC clinical protocols: Adult, Pediatric < 2, Pediatric 2-17 [MG]
JULY 2012
7/26.2012. New protocols for the initial activation and workup of stable and unstable trauma patients were approved at trauma council this week. These will be uploaded to the Web site when available. They both invlude a two view “trauma series” as the default, with the addition of an optional lateral C spine when needed. A revised blunt abdominal trauma protocol has also been approved. [MG]
JUNE 2012
6/26/2012: Outside Image Algorithm. A new algorithm, effective July 1, 2012 is now available here:
6/18/2012: Thoracic Spine Radiographs. When a swimmer’s view is obtained as well as an AP and lateral, the exam counts as a 3 view T spine series [MG].
6/11/2012: Rapid Trauma Survey (RTS) w/o contrast removed from scanner.
6/11/2012: Mass Casualty CT Protocol removed from scanner. Instead use RTS.
6/11/2012. Following the ROTE meeting, the following changes were agreed upon re: FAST Spine: Double oblique FAST Axials bone alg with 18 cm FOV. Table-axial 18 cm FOV Std. Eliminating all the extraneous series (including the labelled ones).
MARCH 2012
3/31/2012. SAFIRE (Siemens Iterative Reconstruction) turned on for most series. This will require some fine tuning in the days and weeks to come. Feedback is encouraged. You can identify when SAFIRE is used for reconstruction, and the strength by looking at the reconstruction kernel on PACS. If the kernel name starts with “I”, then SAFIRE has been used. The number after the slash represents the strength. e.g. “Ker: I70h / 3” means SAFIRE is used, with strength 3.
FEBRUARY 2012:
2/23/12: Interpretation of Outside Exams: Clarification about the new procedure for interpretation of outside exams: The flowchart that has been posted refers to cross-sectional studies that do not have accompanying final reports on ED transfer patients. Studies affected are from the current episode of care (does not apply to historical exams). With respect to plain films, key studies from the current episode of care that do not have accompanying final reports should be dictated as well. We leave it to the discretion of the resident as to the identification of “key studies”, but typically it would include the first and last of a series of related exams (say, sequential chest x-rays, or an unsuccessfully reduced dislocation). An exam that is not likely to be repeated after transfer to HMC would also qualify as “key”. This procedure applies 24/7 and goes into effect on February 27, 2012. [JR]
2/2/2012: Care kV and CTA Problem in obese patients: Due to problems with CarekV selecting 100 kVp for CTA’s (including DRO) in obese patients and awful, noisy images being produced, our CT techs were asked to lookout for this, and to turn CarekV off and manually select 120 kVp in these patients. [MG]
JANUARY 2012
1/25/2012: Gated DRO / PE Studies: By default, technologists will be prospectively gating DRO studies in the ED when the heart rate is > 90 bpm. [MG]
1/23/2012: Increased reference mAs for Trauma CT C Spine. Today the reference mAs on the Siemens scanner was increased form 250 to 300. This was based on phantom testing. Aim was to improve image quality in the upper T spine. Please keep an eye on IQ through the upper T spine, and radiation dose, and provide feedback. [MG]
1/17/12: Gastrointestinal hemorrhage CTA protocol. Added to CT scanners and to CT protocol books. Use this protocol for suspected acute GI bleeding. [MG]
1/7/12: Siemens Abdomen/Pelvis dose. Ref mAs for the abdomen and pelvis CTs corrected to the values specified in recent communications and in the protocol book. eg : 210 for T3. [JG]
1/2/12: DRO PE protocol timing. The delay from start of injection to start of scanning has been increased from 35 secs to 40 secs, to attempt to utilize all the contrast injected and improve visualization of pulmonary arteries. [JG]
DECEMBER 2011
12/29/11: Problems accessing CT Protocols online. There is currently a problem accessing these protocols from some PCS, with an error occuring after you enter your user name and password as requested. This issue is being reviewed to try and make it work seamlessly as it did before some recent changes. [JG]. For now it appears that you need to login by specifying the AMC domain. Work continues to simplify this process.
12/29/11: Double Rule Out PE protocol. We will modify this protocol on the Siemens scanner to start scanning 5 seconds later, which will hopefully provide better contrast enhancement. Log will be updated when change is implemented. [JG]. Updated – see 1/2/12.
12/29/11: Power Outage Tonight. The main power will be down from 8pm – midnight. Much, but not all of our equipment, will work on emergency power during this time. CT1 and the 1.5T MRI will not work during this time. We are continuing to work with the parties involved, but be aware that we may need to prioritize patients to scan and exams to be sent over at the transition times. Save your dictated reports frequently around the transition times, so you don’t accidentally lose a long complex report if your system crashes during the transition. [JG]
12 / 6 11: Coronary CTA Workflow. Document outlining the workflow sent out. This is primarily to assist schedulers, nurses and technologists. Available here. [MG]
NOVEMBER 2011
11/22/11: Critical results reporting. Email from MG to ERad faculty. HMC Radiology Critical Results Reporting Policy is available by clicking here. Refer to 11/1/11. [JG]
11/23/11: Updated discriminatory value for beta-hcg in pregnancy to 1,000 mIU/ml (3rd IS). Search for “beta” or “Discriminatory beta-hcg levels” or “First trimester US”. Page is available here [MG]
11/8/11: HMC Backup (HEB) Resident coverage 11/29-21/1/11. D/t technical problems, the ERad schedule (and other schedules) do not accurately list the HEB resident. Please see the Amion Call (master) schedule instead. This can be accessed by clicking here. For problems, contact the chief resident or their representative (the residents should know how to do this). At this time, the HEB coverage is as follows: 11/29: Brendan McCullough. 11/30 & 12/1: Nick Bodmer. [JG]
11/3/11: Diverticulitis study. Lisa Strate. Please refer to laminated cards at ERad workstation if you identify a patient with suspected diverticulitis, so you can contact the research team at that time. [MG]
11/1/11: Critical results reporting. Search for “Critical Results Reporting” to review the updated policy. Reporting Policy is available by clicking here. [MG]
OCTOBER 2011
10/25/11: MRI policies for pregnant patients reviewed. Policy is available on HMC Hospital Web Site (requires AMC Login and for you to be using an HMC computer). Can be accessed by clicking here. [MG]