by nathangl | Apr 21, 2021 | News
 On March 1, 2020, I released a note that fewer than 10 individuals in Washington state had been diagnosed with COVID-19. As of this writing, more than 386,000 Washingtonians have been infected and 5,500 have died. Nationwide, more than 550,000 Americans have died during this pandemic. The SARS-CoV-2 – an infection unknown to us before last year, has touched everyone in every way possible.
On March 1, 2020, I released a note that fewer than 10 individuals in Washington state had been diagnosed with COVID-19. As of this writing, more than 386,000 Washingtonians have been infected and 5,500 have died. Nationwide, more than 550,000 Americans have died during this pandemic. The SARS-CoV-2 – an infection unknown to us before last year, has touched everyone in every way possible.
We were all worried – and for good reason. We worried about our family, friends, colleagues and ourselves. We worried about our education, clinical skills and ability to learn in an environment that had been disrupted for more than a year and, in many ways, continues to be unfamiliar to us. Somehow, we adapted together – as well as we could, and brought ourselves back to the rhythm of the academic year.
At the beginning of 2020 recruitment season, many of us had no idea what to expect. How were we going to interview candidates? Would the selection of residents ultimately be fair? Would we be able to attract Underrepresented in Medicine (URiM) candidates? Would certain Black and Brown populations be at further risk by asking them to travel to Seattle? Like most other medical schools, the UW SOM decided that all interviews would be conducted virtually, even interviews for its own medical students. This decision – and the unpredictability of the virus – created lots of anxiety.
So, we got to work.
The GME Office, which is traditionally not involved in the recruitment season activities, produced three videos that would capture the essence Seattle for the twenty-something perspective. This could not have been accomplished without the generous support of our clinical departments. The GME Office also organized town halls and networking opportunities for program leadership to discuss best practices for website marketing, communication strategies and diversity recruitment. Some programs developed their own materials to attract candidates who would not be able to visit Seattle.
The Network of Underrepresented Residents and Fellows (NURF) hosted two diversity and inclusion events in an attempt to help all of our programs attract underrepresented and vulnerable minority candidates. NURF even hosted a third, second-look event. These virtual events were successful, attracting hundreds of candidates who would learn more by asking questions and participating in small break-out room conversation.
So, did any of this work?
It did! The UW SOM had one of the best recruitment seasons in the past 15 years. All of our ACGME and non-ACGME programs matched with only one program using the Supplemental Offer and Acceptance Program (SOAP).
Everyone had to make adjustments due to COVID-19, including medical student applicants, the National Residency Match Program (NRMP), program leadership and sponsoring institutions. In spite of the global pandemic, NRMP had the largest number of applications ever and the largest Match on record with 48,700 registrants, an 8.3% increase over 2020.
The UW residency programs offered 285 positions, 48 individual tracks, including a new track called Pediatrics Health Equity. Of the residency positions, 274 matched with only 11 spots eventually matching through SOAP, which resulted in 100% match rate. Forty-six UW medical students matched with our residency programs. Of the 285 who ultimately matched, there were 46 UW medical students, 200 US seniors, 16 IMGs and 12 from osteopathic medical schools.
The UW fellowships offered 163 positions, 34 of which were filled by UW residents. Only 3 positions ultimately did not match.


At UW – and around the country, there was a new focus on diversity and inclusion which proved to attract and match many Black and Hispanic, as well as female candidates According to a recent NY Times article (After A Year of Toil, Elite Universities Welcome More Diverse Freshman Classes, April 17, 2021), the death of George Floyd created a national consciousness of racial injustice and placed a greater value on diversity. As a result, early data suggests that many elite undergraduate universities admitted a higher proportion of first generation, lower income and traditionally underrepresented students.
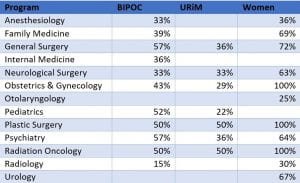
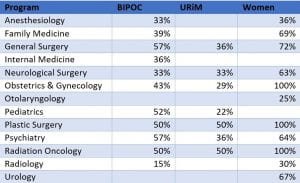
Although the NRMP does not traditionally release diversity data for the Match, it appears that medical schools also followed this trend. It appears that the University of Washington did. Many of our clinical programs proudly reported on their success with BIPOC, URiM and women candidates:
Hopefully, we can sustain this trend, not just for this moment. Hopefully, we will be able to preserve this social awareness and continue to expand diversity in our pools of candidates who will eventually apply for, matriculate to and graduate from medical schools around our country. It will be important for UW to continue to create a healthy and safe learning and working environment for BIPOC medical students and trainees, cultivating our efforts of equity, hiring more diverse faculty and creating spaces where everyone can learn and thrive.
Overall, this Match year was a very good one. Thank you all for your individual and group efforts.
Byron D. Joyner, MD, MPA
Vice Dean and Designated Institutional Official (DIO)
Graduate Medical Education, UW Medicine
by nathangl | Mar 19, 2021 | Announcements, GME News & Notes, News
Dear GME Community,
Happy Match Day! This is our second “News and Notes” post, including bi-monthly updates about members of our community, policy updates, program changes, events of interest, and other updates. If you have feedback, and/or information or events that you would like us to include in future posts, please send them to me at hamrac@uw.edu.
Cindy

Cindy Hamra
Assistant Dean of GME
People
- Barbara Jung, Chair of the Department of Medicine, joins the presidential line up for the American Gastroenterological Association (AGA). She will serve as vice president, president-elect and will become president in 2023. She will be the 4th woman holding this office.
- Jennifer Best, Associate Dean for GME and Associate Program Director for the Internal Medicine Residency Program, and Hadar Duman, GME Director of Accreditation, joined colleagues from the University of Colorado School of Medicine and University of New Mexico School of Medicine to present “Special Reviews: When You Still Haven’t Found What You’re Looking For” at the 2021 ACGME Conference in February
- Estell J. Williams, Assistant Professor, Department of Surgery, and General Surgery Residency Program alum, received the 2021 Distinguished Service Award for Community Service and Volunteerism, in celebration of Martin Luther King, Jr.’s legacy. The award is sponsored by the UW Health Sciences Administration & University of Washington Medical Center.
- John Choe, Associate Professor, General Internal Medicine, and Associate Program Director in the Internal Medicine Residency Program, has been elected to the governing council for the Association of Program Directors in Internal Medicine (APDIM), part of the Alliance for Academic Internal Medicine (AAIM).
- Judy Pauwels, Associate Director of Program Development in the UW Family Medicine Residency Network, is the recipient of the Senior Women Faculty Mentor Awardee from the Dean’s Standing Committee on Women in Medicine.
Policies
- The Graduate Medical Education Committee (GMEC) approved a new Chief Resident/Fellow Policy at the March meeting, which is posted on the Policies and Procedures page.
- The New Program Application for GMEC Approved Non-Accredited Fellowship Programs was revised by the GMEC-Approved Non-ACGME Fellowship (GAF) Programs Committee in February and is available for new programs on the Non-ACGME Programs Resources page on the GME website. In addition to the revised application, the GAF Committee also developed a new Department Chair Letter of Support letter template for new non-ACGME program directors. Questions about the application can be directed to Gabrielle Pett at nathangl@uw.edu.
- The Residency and Fellowship Position Appointment (RFPA) Agreement 2021-2022 is now posted to the Policies and Procedures page.
- A friendly reminder that pursuant to the MedHub User Access Controls Policy, requests for MedHub accounts must now be requested via forms posted to the MedHub page of the GME website.
- The ACGME has released new Institutional Requirements, which will take effect July 2021.
Program Information
- Today is Match Day for the NRMP Main Residency Match. Please join us in congratulating our residency programs that filled all 285 available positions offered in this year’s Match. You can read the NRMP’s Press Release here. We will share a larger update on UW’s Match results in the coming weeks.
- The GMEC has approved the following new ACGME program director appointments. All are awaiting ACGME approval:
- Clinical Cardiac Electrophysiology: Dr. Nazem Akoum, replacing Dr. Kristen Patton
- Epilepsy, Dr. Jeffrey Tsai, replacing Dr. Norman So
- Hematopathology: Dr. Dan Sabath, replacing Dr. David Li
- Developmental-Behavioral Pediatrics, Dr. Emily Myers, replacing Dr. Samuel Zinner
- The GMEC also approved Dr. Travis Nelson, as the new Program Director for Pediatric Dentistry, replacing Dr. Zheng Xu
Events of Interest
- Registration for the Spring Program Director Development Series is now open. If you haven’t yet signed up to join us, please register before noon on March 29.
- Join us for our Program Administrator Meeting, on Tuesday, April 13. Topics include Annual Program Evaluation (APE) best practices and presentations from the Continuous Process Improvement (CPI) contest. Event details can be found here.
- Other GME Events can be found on our calendar: https://sites.uw.edu/uwgme/calendar/
COVID Updates
- Reopening Vaccine First-Dose Appointments to Eligible 1A and 1B1 Employees: With a third COVID-19 vaccine now approved and vaccine supply increasing nationwide over the next few months, we are pleased to begin scheduling first-dose vaccinations for employees who meet the Washington State Department of Health eligibility criteria. Eligible employees are those in Phase 1A or 1B tier 1. This includes healthcare workers at high risk for COVID-19 infection, first responders, people who live or work in long-term care facilities, anyone 65 and older, people 50 and older who also live in a multigenerational household, and educators, staff and child care workers in pre-K, K-12 or daycare settings. If you are eligible for COVID-19 vaccination, please visit the UW Medicine employee COVID-19 vaccine site to schedule your appointment.
- Travel restrictions for UW Medicine employees remain in place, even for those who have already received the vaccine. This includes work-related travel for conferences and meetings. Non-essential personal travel also is strongly discouraged until further notice.
- Scheduling for COVID Moonlighting shifts is transitioning from the GME Office back to the services effective shifts starting 3/22/2021. Residents with questions can still contact Cindy Hamra (hamrac@uw.edu) for help navigating.
- UW COVID-19 Employee Emergency Fund: The roll-out of the coronavirus vaccine has brought new hope to all of us. At the same time, members of our community continue to feel a variety of impacts on their lives. For many, the financial strain of this time is significant. We want to remind everyone that the UW COVID-19 Employee Emergency Fund (EEF) remains available to employees most in need. In addition, we know that changes in the availability of child care resources and the addition of remote learning have at times felt overwhelming. To help ease some of these challenges, we are excited to announce that the Employee Emergency Fund is now offering an additional child care supplement.
- We continue to update our guidance for residents/fellows and programs on the GME COVID page: https://sites.uw.edu/uwgme/covid-19-updates-gme-community
Progress, Activities and Resources
- Bias Incident Reporting Tool Our commitment to a culture of inclusivity is shaped by the actions we take to recognize injustice and address and correct it where it occurs. One such measure, now available for the UW Medicine community, is the Bias Incident Reporting Tool, created and maintained by the UW Medicine Bias Response Team. This tool offers a mechanism for all community members to safely report incidences of bias and misconduct, and to receive a clear and streamlined response.
- 2021 PAAC Continuous Process Improvement Contest: Do you have the perfect tracking sheet for leave or trainee publications? The perfect CCC process or excellent MedHub evaluations? A great idea for how to innovate GME through program improvement? Send in a submission to the 2021 PAAC Continuous Improvement Contest! Send a brief summary (250 words) of what tool you’re submitting, the issue it addresses, and any examples to the PAAC at paac@uw.edu by March 26.
- 2022 ACGME Awards Nominations Open The ACGME recognizes notable designated institutional officials, program directors, residents and fellows, and institutional and program coordinators for their outstanding work and contributions to graduate medical education through its Awards Program. Nomination materials are available in the Awards section of the ACGME website. The deadline for nominations is March 24, 2021, at 5:00 p.m. Central.
- UW Human Resources is launching an Advisory Committee on Work-Life. Formed at the recommendation of the COVID-19 Caregiver Task Force, this group will help guide the University’s continued response to COVID-19 caregiving challenges and shape post-pandemic work-life initiatives. UW Medicine will be represented in the committee by Anne Browning, School of Medicine Assistant Dean for Well-Being and Aimee Buckius, UW Medicine Human Resources. To help us understand the unique and nuanced needs of our community, please take a few minutes to share your thoughts with us.
- The American Hospital Association, in partnership with ACGME, the National Association of Medical Staff Services, and the Organization of Program Director Associations and others, recently released an updated version of the Verification of Graduate Medical Education Training (VGMET) Designed to streamline and standardize the residency verification process and meet hospital credentialing needs, the template letter and form provide the necessary information to meet credentialing needs while reducing the need for residency programs to complete multiple requests for information.
by nathangl | Mar 3, 2021 | News
 The early 20th Century was the birth of Black History Month. It began as a proposal of only a week. Carter G. Woodson, an American historian, author, journalist, and the founder of the Association for the Study of African American Life and History, started what was to become a movement. He announced that the second week of February would be Negro History Week. HIs choice of February is not well-documented, but some historians believe that the inspiration was because February was the birth months of both Abraham Lincoln and Fredrick Douglas. Mr. Woodson’s extensive work on the Journal of Negro History, which took 10 years to complete, made him realize that the “recognition and importance” of Black people in this country was deserving of a larger audience.
The early 20th Century was the birth of Black History Month. It began as a proposal of only a week. Carter G. Woodson, an American historian, author, journalist, and the founder of the Association for the Study of African American Life and History, started what was to become a movement. He announced that the second week of February would be Negro History Week. HIs choice of February is not well-documented, but some historians believe that the inspiration was because February was the birth months of both Abraham Lincoln and Fredrick Douglas. Mr. Woodson’s extensive work on the Journal of Negro History, which took 10 years to complete, made him realize that the “recognition and importance” of Black people in this country was deserving of a larger audience.
I couldn’t agree with him more.
All of us need to pause and appreciate the many gifts that Black Americans have given to this country, in shackled times and in times of unshaken pride. The fact that the gifts, given by Black Americans, have traditionally gone unrecognized by history is what should make us all appreciate more the injustice Blacks have suffered by the erasure of individual and collective Black contributions.
February is the annual celebration of not just those African Americans who have made specific contributions but to all African Americans who have been downtrodden by not being appreciated. Years of not appreciating our collective lives and losses have created a hurt that has affected all of us.
As I look toward the New Year and reflect on the many past, present and planned graduate medical education (GME) initiatives for improving diversity at the UWSOM, I think of the many ways in which GME has attempted to nurture our Black residents and fellows and, as much as possible, help them in their endeavors and honor their presence while they are here.
In many ways, our Black trainees have had the strength and sheer will to make many of our activities of appreciating Black contributions possible. The Network of Underrepresented Residents and Fellows (NURF) started nearly 13 years ago from the request of 4 Black women graduates of UW medical school. That once small and inchoate group has continuously thrived and is fully recognized and appreciated by the entire UWSOM as dynamic, energetic and inclusive. Even during the pandemic, the group has been busy. NURF led the recruitment effort this year with two diversity Town Halls for all specialties and followed that up with a recent Second Look for URiM and diverse candidates. These virtual meetings have been organized, informative and well-attended.
NURF has also partnered with the Housestaff Quality & Safety Committee (HQSC), another resident-run, multi-specialty organization in which members are interested in quality and patient safety issues and initiatives. NURF and HQSC members have created the Joint Conference in QI & Health Care Equity which, with the involvement of medical directors and other faculty, has created substantial projects around health and equity for marginalized patient populations.
GME is collaborating with the Office of Healthcare Equity to host Black Men In White Coats this week. The founder of this movement, Dr. Dale Okorodudu will join us to describe his work in supporting Black families, diverse communities and all medical schools in celebrating Black academic achievement so that the process of recruiting and retaining more Black men in medical schools around our country is a reality. Black Americans represent about 13% of the population but fewer than 4.4% of all medical trainees and 2/3 of those are Black women. We have much work to do.
I celebrate the work that we have done, not just in February but throughout the year for our Black housestaff. I celebrate the work they have done and continue to do with their white and Brown allies to make the future better for us all. As I look toward 2021 – and the rest of our lives, I want us to appreciate Black achievement every day and celebrate Black history which is part of our collective American history.
Byron D. Joyner, MD, MPA
Vice Dean and Designated Institutional Official (DIO)
Graduate Medical Education, UW Medicine