by amande | Feb 22, 2024 | Announcements, Events, GME News & Notes, News

Dear GME Community,

Cindy Hamra Associate Dean, GME
Please join me in welcoming our new Appointment Manager, Shinetra Pryor who joined the GME Team on January 31st! Shinetra is joining us from the UWSOM Geriatric and Palliative Care fellowship programs where she was the Program Administrator. Shinetra has worked within UW Medicine since 2007 and joins GME with a wealth of knowledge. She was also recently awarded the Recipient of the inaugural Department of Medicine Outstanding Staff Award!
Thank a Resident Day is Friday February 23rd. Thank a Resident Day is sponsored by the Gold Humanism Honor Society and takes place each year to collectively show gratitude and appreciation for residents and how integral they are to the healthcare team. We’re planning GME Outreach events and encourage programs and departments to plan to celebrate as well!
Finally, in February, we celebrate Black History Month. Since there are so many wonderful resources, we’ve added a section in the newsletter directing to many of them.
Thanks,
Cindy

Black History Month
- The Office of Healthcare Equity is an excellent resource for talks and training on the principles of equity, diversity, inclusion and justice. The Huddle Black History Month page provides digital assets to take part in this month’s celebration, as well as learning resources for all employees and self-care resources for Black employees.
- Black History Month: Celebration, Reflection and Action: Read the message from UW Medicine leadership celebrating the contributions of our Black colleagues and learn how our health system is working to dismantle healthcare inequities.
- We invite you to read this excellent article on the recent history of black physicians in Seattle and on George Counts, the first Black professor in the UW Department of Medicine and an important leader in Public Health and mentor to many.
- Celebrating Black History Month: Honoring Ancestors, Looking Forward from The Huddle explores themes of history, art, equity and community and features Ivana Thompson, Associate Chair of Justice, Equity, Diversity and Inclusion in the Department of Obstetrics & Gynecology.
- Read more on President Cauce’s blog post and explore ways to engage through The Whole U.
Policies and Processes
- The AAMC, in collaboration with the ACGME, is administering the AAMC Resident Readiness Survey, a process of collecting and sharing information back to medical schools about their graduates’ readiness for GME. Program directors currently training any PGY-1 resident who is a 2023 graduate from any of the 174 participating medical schools have been invited to respond to the Resident Readiness Survey administered via GME Track. We encourage program directors who have not completed entering the information to do so before February 23, 2024. They should log into GME Track, click the Resident Readiness tab at the top of the screen.
- Residency and Fellowship Position Appointment (RFPA) Agreement for 2024-2025: the AY25 RFPA was approved by GMEC on January 11 and is now available on the Policies and Procedures, Current Residents and Fellows, and Prospective Residents and Fellows pages of the GME website.
- The GMEC has approved appointment of the following new Non-ACGME program directors:
- Brittany Barber, Head and Neck Oncology and Microvascular Reconstruction Fellowship
- Craig Birgfeld, Pediatric Craniofacial Surgery
- Meghan Flanagan, Breast Oncology Surgery
- The ACGME has a weekly e-Communication. If you wish to receive it, email ACGMECommunications@acgme.org.
Events of Interest
- GME Lunch & Learns
- February 15: Washington Physicians Health Program (WPHP), slides and recording are now available
- March 21: Annual Program Evaluations (APEs)
- April 18: GMEPAC AY26
- GME Event Follow up: Navigating Parental Leave During Residency and Fellowship – recorded virtual event held on February 6, 2024 has been posted on the GME website, including several resources. Bre Leatherman is available to answer any questions you may have.
- The first session of our Cultivating Skills in Feedback and Critical Conversations Education Series is Tuesday February 27 from 11:30am to 1:00pm. In response to your feedback, we will be offering an in person session with lunch provided and a virtual option. The focus of the 2/27 session will be: Why Feedback Matters – The Impact of Feedback Culture and Remediation on Programs, Learners and Leaders. Program directors, associate program directors, program administrators and faculty are welcome. For planning purposes, please RSVP by Friday, 2/16. Please reach out to Amanda Easton and Jenn Johal if you have questions and we hope to see many of you there.
- We are excited to announce a comprehensive Four-Part Leadership Lecture Series designed specifically for residents and fellows! Each month, we will delve into crucial areas that shape effective leadership in the medical profession, presented by experts in the field. Mark your calendars and join us! Registration will open in February. Please see the January 18 email from Jennifer Best for more information.
- Upcoming Program Director Development Series: This is a reminder to registration for our Spring Program Director Development Series on March 19th or April 8th. Please register at: https://sites.uw.edu/uwgme/pdds-registration/ .This season we are excited to offer two transformative sessions dedicated to the advancement of resident and fellow well-being and the refinement of recruitment program strategies. All sessions will be held on Zoom.
- Registration for the ACGME Meaning in Medicine 2024 Annual Education Conference is open! The conference is in Orlando, FL March 7-9, 2024. Support for meeting attendance is ensured by the clinical chair in every new Program Director Appointment Letter. Several members of the UW GME team will be attending the conference and we would like to know if you’ll be attending and/or presenting. Once we have a sense of UW representation, we are hoping to find time for UWSOM colleagues to get together for an onsite lunch or photo. Please contact Amanda Easton if you or members from your department will be in attendance.
- The UWSOM is sponsoring the 2024 Graduate Medical Education (GME) Summit. The focus will be collaborating to address workforce needs within the WWAMI region and beyond. Registration for the Summit is now open! Join us on April 25-26, 2024, in Anchorage, Alaska.
- Space still available for CRISP: CLINICAL RESEARCH INTENSIVE SUMMER PROGRAM: Applications are still being accepted for this new course designed to provide clinical investigators with hands-on experience in key clinical research skills to accelerate their career development. The program runs July 8–26, 2024 at the Fred Hutch Cancer Center campus in Seattle. A draft daily curriculum may now be viewed on the website under “Class Schedule & Draft Daily Topics.” Read more here.
- Other GME Events can be found on our calendar.
Projects and Resources
 Please review the GME Annual Program Timeline for important dates for the months of February and March.
Please review the GME Annual Program Timeline for important dates for the months of February and March.- On February 14, a new safety event reporting tool called Safety Net will replace Patient Safety Net (PSN), a legacy system that has been in use at UW Medicine for nearly 20 years. There is now an icon for Safety Net on all UW Medicine desktop computers for easy access and all new reports should be entered using Safety Net. Safety Net is an online reporting tool that will help us improve the process of submitting and tracking safety reports so that we can continue to prioritize the safety of our patients, staff, faculty and trainees. For a detailed guide on using the system, please view the instructional video on ‘How to enter an event report in the Safety Net System.’ Safety Net seamlessly integrates reports from Risk Management and Patient Relations thanks to the collaborative effort of teams across UW Medicine. The Safety Net User Resource Page includes training materials, online support and transition plans.
- 2025 ACGME Awards: Nomination materials are available on each award’s page in the Awards section of the ACGME website. All nominations are due March 27, 2024. Please reach out to the GME office if you plan to submit an application.
- Please remember that the UW Medicine Bias Reporting Tool is a place to share incidents of bias including racism, sexism, ableism, discrimination of any form or other behaviors that do not reflect the prioritization of inclusion and equity expected in all areas of our community. The GME Concern Reporting tool is also available to members of the GME community to report concerns about the learning environment.
- The ACGME’s Back to Bedside initiative is designed to empower residents and fellows to develop transformative projects that foster meaning and joy in work and allow them to engage on a deeper level with what is at the heart of medicine: their patients. This initiative supports resident- and fellow-directed innovations. Proposals are due by April 22, 2024. Learn More
- Please review “Access to UW Medicine Care for Employees” from The Huddle for information about help for UW Medicine employees and their families to gain better access to UW Medicine facilities and providers.
- The GME Office is supporting a project called the Names & Pronunciations Initiative, which aims to not only highlight the importance of name pronunciations, but also improve communication by providing physical badges (for those who want one) which include users’ written phonetic name pronunciation. Anyone interested in learning more about the project or who wants to order a pronunciation badge can do so here: https://www.names-pronunciations-initiative.com/. If you have any questions, please email Sudiptho (UW MS4) at sudiptho@uw.edu.
People
- Maheetha Bharadwaj, Urology resident, is featured in “Is it Normal to Wake Up to Pee in the Middle of the Night?” from Parade.
- Katherine Bennett, Geriatric Medicine Program Director, is senior author of “Fumbling the handoff—Exploring the transition experiences of program directors in geriatric medicine” in the Journal of the American Geriatrics Society.
- The UW School of Medicine Colleges Program in the MD program teaches foundational clinical skills, coaches developing physicians, and fosters meaningful relationships and sense of community for UW medical students across the WWAMI region. In July 2024, the Colleges program on the Seattle campus will be expanding from 2 to 4 Colleges and is proud to be welcoming two outstanding leaders from the DOM as new College Heads. This includes Gaby Berger, Internal Medicine Associate Program Director.
- Jennifer Best, Associate Dean for GME (Education and Accreditation), is senior author of “The DIO Needs a Cabinet: Identifying and Supporting Designated Institutional “Others” in Graduate Medical Education” in the Journal of Graduate Medical Education.
- Kelley Branch, Cardiovascular Disease Associate Program Director, and Jeff Probstfield, professor (Cardiology) are co-authors of “The Cost-Effectiveness of Rivaroxaban Plus Aspirin Compared with Aspirin Alone in the COMPASS Trial: A US Perspective” in the American Journal of Cardiovascular Drugs. Dr. Branch is also co-author of “Cardiovascular and renal outcomes with varying degrees of kidney disease in high-risk people with type 2 diabetes: An epidemiological analysis of data from the AMPLITUDE-O trial” in Diabetes, Obesity and Metabolism.
- On the latest episode of “Beyond the White Coat,” AAMC President and CEO David J. Skorton, MD, talks with Justin Bullock, MD, MPH (Nephrology fellow), and Yunyu Xiao, PhD, about the stigmas that surround mental health in the medical profession and how those stigmas trickle down into patient care. The episode is available wherever podcasts are streaming and can also be accessed on YouTube. Listen Now. He has also been selected as the new co-director of Docs with Disabilities Initiative, joining the 2024-26 leadership team. Docs with Disabilities Initiative is a leader for disability inclusion in health professions training globally. Learn more on the Department of Medicine news site.
- Richard Cheng, Advanced Heart Failure/Transplant Cardiology Program Director, is quoted in “Demystifying cardiac sarcoidosis” in Medscape.
- Recognizing outstanding leadership since 2006, the Thorud Leadership Award is the highest leadership honor at the University of Washington. Congratulations to this year’s nominees from the Department of Medicine, Debra Cherry, Occupational and Environmental Medicine Program Director (General Internal Medicine), William Lombardi, CHIP – Advanced Hemodynamic Care and Complex Coronary Interventional Program Director (Cardiology) and Susan Wong, associate professor (Nephrology).
- Jason Deen, associate professor of pediatrics and medicine (Cardiology) has been appointed chairperson of the American Academy of Pediatrics’ Committee on Native American Child Health (CONACH). Dr. Deen, a current member of CONACH, is a pediatric cardiologist, vice chair for equity, diversity and inclusion in the Department of Pediatrics and director of the UWSOM Indian Health Pathway.
- Sara Gunby, fellow (Gastroenterology) is referenced in “Smoking and Drinking Up the Risk for Diverticulitis” in Medscape.
- Jonathan Harper, Endourology Program Director, is featured in “Millennials, Listen Up: No. 1 Tip to Prevent Kidney Stones” from Right as Rain.
- Whitney Harper, program operations specialist (Internal Medicine Residency) is co-author of “Optimizing the Internal Medicine Residency Recruitment Process: A National Survey of Program Directors and Next Steps” in the American Journal of Medicine.
- Ramesh Iyer, Radiology Vice Chair of Education, has been appointed as Section Chief of Pediatric Radiology and Site Director for Seattle Children’s Hospital.
- Lily Jeong, incoming fellow (Nephrology) is a 2024 recipient of the American Society of Nephrology Loan Mitigation Pilot Program. This program aims to reduce the loan burden of future nephrology leaders. Dr. Jeong completed medical school and is currently in her last year of residency at UW in the clinician educator track.
- Barbara Jung, Department of Medicine chair, is featured in “’GI is Everything’: An Interview with AGA President Dr. Barbara Jung” from Op-Med Doximity. She is also author of the op-ed “Why Are We Letting Insurers Dictate Patient Care?” from MedPage Today.
- Andrew Ko, Neurological Surgery Program Director, is featured in “Analysis: Several companies are testing brain implants — why is there so much attention swirling around Neuralink? Two professors unpack the ethical issues” from The Conversation.
- Andrew Koth (Pediatric Critical Care Medicine Program Director), Emily Rhee (Pediatric Critical Care Medicine Associate Program Director), and Jessica McDade (fellow) are featured in “A Day in the Life of Employees Fostering Equity, Diversity and Inclusion” from The Huddle.
- Hannah Linden, Hematology and Oncology Associate Program Director, is co-author of “Activity and safety of enobosarm, a novel, oral, selective androgen receptor modulator, in androgen receptor- positive, oestrogen receptor-positive, and HER2-negative advanced breast cancer (Study G200802): a randomised, open-label, multicentre, multinational, parallel design, phase 2 trial” in The Lancet.
- Heather McPhillips, UWSOM Associate Dean for Curriculum, has been elected Chair of the ACGME Pediatric Residency Review Committee to begin serving on July 1, 2024.
- Susan Merel, associate professor, Gabrielle Berger, Internal Medicine Associate Program Director, Amanda Shepherd, Internal Medicine Associate Program Director, Lindsay Gibbon, clinical assistant professor (General Internal Medicine) and Patricia Kritek, SOM Vice Dean of Faculty Affairs, are co-authors of “An Embedded Curriculum to Teach Critical Incident Debriefing to Internal Medicine Residents” in the Journal of Graduate Medical Education. Lead author is former chief resident James Wykowski.
- Leo Morales, Assistant Dean for Healthcare Equity and Quality, is quoted in “More states offer health care coverage for certain immigrants, noncitizens” from San Jose Mercury News.
- Paul Nghiem is the founding chair of the Department of Dermatology as of March 1, 2024.
- Johnnie Orozco, Hematology and Oncology Associate Program Director, and Phuong Vo, associate professor, are co-lead authors, and Brenda Sandmaier, professor (Hematology and Oncology) is senior author of “Targeted Radiation Delivery before Haploidentical HCT for High-risk Leukemia or MDS Patients Yields Long-term Survivors” in Clinical Cancer Research. Department of Medicine co-authors are Ajay Gopal and Damian Green. The paper was also featured in the American Society for Transplantation and Cellular Therapy Science Highlights.
- Meena Ramchandi, Infectious Diseases Program Director, is featured in “UW Medicine: King County sees ‘great increase’ in syphilis cases following national trend” from My Northwest.com.
- Coralynn Sack, Occupational and Environmental Medicine Associate Program Director, is lead author of “Airway Tree Caliber and Susceptibility to Pollution-associated Emphysema: MESA Air and Lung Studies” in the American Journal of Respiratory and Critical Care Medicine. Department of Medicine co-author is Joel Kaufman.
- The Huddle recently featured an article, New Program Provides Rural Surgery Training for Residents. General Surgery R4 Hannah Wild is the first resident to participate in the track.
- The Department of Surgery Newsletter ‘Surgery Synopsis’ features many voices of the GME community, including Program Directors, trainees, and program staff. Check out the Winter 2024 issue.
- Crystal Brown, assistant professor (Pulmonary, Critical Care and Sleep Medicine) is lead author and Bessie Young, Vice Dean of Equity, Diversity, and Inclusion, is senior author of “Physician Perspectives on Addressing Anti-Black Racism” in JAMA Network Open. Department of Medicine co-authors are Arisa Marshall, Kristine Cueva and Erin Kross.
- Michelle Zhang, R3, was an invited presenter at the Best of SWOG research webinar on her research, evaluating the relationship between obesity and survival in patients with acute myeloid leukemia treated on the SWOG 1203 clinical trial. Read more on the Department of Medicine news site.
by amande | Feb 9, 2024 | Announcements, News

Byron Joyner, MD, MPA
I am very excited about our new, 6-year GME strategic plan We’re excited about this plan, which shapes our priorities, guides our work and allows us to request resources. It’s also an important way for GME to communicate to our stakeholders about the breadth and depth of our work on behalf of this community. For the February DIO Blog, I’ve invited Cindy Hamra, Associate Dean for GME to share an update on the GME Strategic Plan. We’ll continue to share updates a few times each year to keep you updated on our progress.
Byron Joyner, MD, MPA
Vice Dean for Graduate Medical Education, Designated Institutional Official

Cindy Hamra, JD, MA
In August, we introduced the new GME Strategic Plan, which will be effective from July 2023 through June 2029. This is our fourth strategic plan since I have been in the GME Office and it’s by far been our most inclusive and robust process. We learn from each iteration.
The process of developing the final version of our strategic plan took about 11 months and included a SWOT survey to GME stakeholders, data analysis by a group of GME team members, reviewing guiding documents including ACGME requirements, the UW Medicine Strategic Plan, and the Office of Healthcare Equity Blueprint. We identified several themes and framed them according to our strategic values, which have guided our work since 2019. Although contexts may change, our strategic values have not. A snapshot of the resulting plan looks like this:
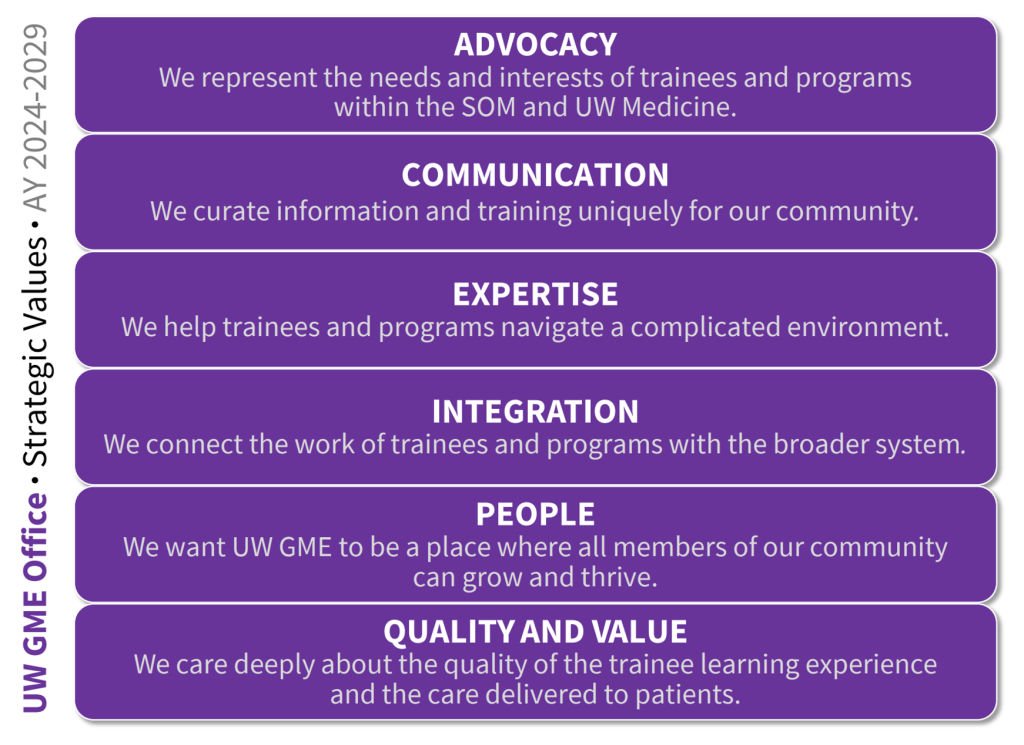
We’ve shared this resulting plan with many groups since July 2023, including this video. Our team has simultaneously been working on implementation – planning out the projects and work that we want to accomplish. I’m excited to share some of the many projects that are already complete or underway!
| Strategic Value |
Strategic Initiative |
Project / Work |
| Advocacy |
Improve communication to programs and trainees regarding grant funding impacts |
Develop GME Grant Funding Policy – complete |
| Communication |
Leverage collective expertise of senior GME educators and share educational / administrative best practices |
Develop template for new Vice Chair for Education (VCE) roles that can be used by departments in oversight of the educational mission – complete |
| Communication |
Leverage collective expertise of senior GME educators and share educational / administrative best practices |
Engage departmental VCE to inform GME practices and community education and enhance program support – in progress
|
| Communication |
Gather community for relationship building to enhance well-being in the workplace |
GME Office Professional Development Discussion Series – in progress
|
| Expertise |
Strengthen support for and oversight of non-ACGME programs |
Develop Visa Matrix for departments to navigate requirements for fellows in faculty and non-faculty titles – complete |
| Integration |
Proactively align educational structures with UW Medicine’s clinical strategy |
Patients experiencing incarceration eLearning module – in progress
|
| Integration |
Proactively align educational structures with UW Medicine’s clinical strategy |
HealthierHere eLearning module – in progress |
| People |
Build trust / credibility with trainees at-large |
Enhance mechanisms for receiving and responding to trainee feedback (e.g., special reviews, chief residents listening sessions, trainee forum) – in progress |
The table above reflects a fraction of the work that is underway. We welcome input from and participation by our community. If you’re interested in joining this work, feel free to reach out to me.
We’ll continue to share updates with you for the duration of the plan. In the meantime, feel free to reach out if you have questions or feedback. We believe this work will make our GME community stronger and the learning experience better for our residents and fellows.
Cindy A. Hamra, JD, MA
Associate Dean, Operations & Administration
Graduate Medical Education| UW Medicine
by amande | Jan 19, 2024 | Announcements, Events, GME News & Notes, News

Dear GME Community,

Cindy Hamra Associate Dean, GME
Happy new year! There are lots of reasons to celebrate this month including Dr. Byron Joyner, our Vice Dean and DIO receiving the 2024 Presidential Citation from the American Urological Association, and Dr. Claire Oduwo, Psychiatry resident, receiving the UW Medicine Martin Luther King Jr. Community Service Award in 2024.
Please plan ahead for Thank a Resident Day, which will be Friday February 23rd. Thank a Resident Day is sponsored by the Gold Humanism Honor Society and takes place each year to collectively show gratitude and appreciation for residents and how integral they are to the healthcare team. We’re planning GME Outreach events and encourage programs and departments to plan to celebrate as well!
Please remember that the UW Medicine Bias Reporting Tool is a place to share incidents of bias including racism, sexism, ableism, discrimination of any form or other behaviors that do not reflect the prioritization of inclusion and equity expected in all areas of our community. The GME Concern Reporting tool is also available to members of the GME community to report concerns about the learning environment.
Cindy
Policies and Processes
- Residency and Fellowship Position Appointment (RFPA) Agreement for 2024-2025: the AY25 RFPA was approved by GMEC on January 11 and is now available on the Policies and Procedures, Current Residents and Fellows, and Prospective Residents and Fellows pages of the GME website. A communication about the updated agreement was sent to current residents, fellows, program directors and program administrators on January 16. Programs currently interviewing candidates for the 2024-2025 academic year must provide candidates with a copy of the updated agreement.
- The GMEC approved revisions to the following policies at the January meeting. All are posted on the Policies and Procedures page of the GME website.
- Drug Enforcement Administration (DEA) Registration Policy: Minor updates were made to the DEA Registration Policy including adding a Purpose statement and updating the attestation requirement for opioid management training, which was communicated to programs in May 2023.
- Resident and Fellow Evaluation Policy: Has been revised to include non-ACGME fellowships and NST programs. A new Definitions section has been added, and the Policy section reorganized to clarify PD responsibilities and evaluation processes. Significant updates were made to the Semiannual and End of Year Evaluation sections, with a specific focus on NST trainees. The Resident Evaluation Management and Access section was renamed and updated, and outdated guidelines were removed from the attachments.
- A reminder that residents and fellows are essential personnel who are expected to report for duty; please see guidance from Residency and Fellowship Position Appointment (RFPA) Agreement 2023-2024 and Executive Order 27: Suspended Operations Policy
Events of Interest
- GME Lunch & Learns
- January 18: ACGME Surveys, slides and recording are now available
- February 15: Washington Physicians Health Program (WPHP)
- March 21: Annual Program Evaluations (APEs)
- We are excited to announce a comprehensive Four-Part Leadership Lecture Series designed specifically for residents and fellows! Each month, we will delve into crucial areas that shape effective leadership in the medical profession, presented by experts in the field. Mark your calendars and join us! Registration will open in February. Please see the January 18 email from Jennifer Best for more information.
- Navigating Parental Leave for Resident & Fellow Physicians will be Tuesday, February 6th from 6:30-7:30pm via Zoom. Please see the agenda. Register at: https://sites.uw.edu/uwgme/event-registration/. Registration closes February 2. If you can’t make it, a recording will be posted to the Housestaff Events webpage.
- Registration for the ACGME Meaning in Medicine 2024 Annual Education Conference is open! The conference is in Orlando, FL March 7-9, 2024. Support for meeting attendance is ensured by the clinical chair in every new Program Director Appointment Letter.
- The UWSOM is sponsoring the 2024 Graduate Medical Education (GME) Summit. The focus will be collaborating to address workforce needs within the WWAMI region and beyond. Registration for the Summit is now open! Join us on April 25-26, 2024, in Anchorage, Alaska.
- Please save the date(s)! The GME Office is pleased to invite program leadership (PDs, APDs, PAs) to participate in GME’s 2024 Educational Series: Cultivating Skills in Feedback and Critical Conversations. See 11/9 email from Cindy Hamra for more information.
- Other GME Events can be found on our calendar.
Projects and Resources
 Please review the GME Annual Program Timeline for important dates for the months of January and February including: Milestones mid-year reporting, semi-annual Procedures Certification entry in MedHub, ACGME Annual Survey preparation, SF Match registration (for applicable programs), and kickoff of activities for the annual onboarding season.
Please review the GME Annual Program Timeline for important dates for the months of January and February including: Milestones mid-year reporting, semi-annual Procedures Certification entry in MedHub, ACGME Annual Survey preparation, SF Match registration (for applicable programs), and kickoff of activities for the annual onboarding season.- Washington State Paid Family & Medical Leave (PFML) premium rates will decrease for UW personnel whose work is performed in the state of Washington. More specifically, the premium rate for the PFML program will decrease from 0.8% to 0.74% of your gross wages up to $168,600 of taxable income. This is paired with a change in the employee–employer split for PFML, with the employee’s contribution decreasing to 71.43%. These changes will be reflected in your January 10, 2024, paycheck. To calculate your 2024 PFML premium contribution and to learn more about PFML benefits, please visit wa.gov. More information about the premium update can be found at https://paidleave.wa.gov/updates/.
- 2025 ACGME Awards: Nomination materials are available on each award’s page in the Awards section of the ACGME website. All nominations are due March 27, 2024. Please reach out to the GME office if you plan to submit an application.
- The ACGME’s Back to Bedside initiative is designed to empower residents and fellows to develop transformative projects that foster meaning and joy in work and allow them to engage on a deeper level with what is at the heart of medicine: their patients. This initiative supports resident- and fellow-directed innovations. Proposals are due by April 22, 2024. Learn More
- Our GME PLA team is hoping to make strides in communication and improving the process for our community in several ways:
- We created a new, simplified introduction video for the PLA process as a whole here.
- We want to make sure the barriers to completing a rotation request or PLA are as low as possible. If you could please fill out the linked survey and provide feedback it would be helpful and allow us to improve the process.
- Please review the email from Chris Gibson sent on 12/19 for data on expiring PLAs.
- Please review “Access to UW Medicine Care for Employees” from The Huddle for information about help for UW Medicine employees and their families to gain better access to UW Medicine facilities and providers.
- The UW Office of Global Affairs is excited to announce that effective January 1, 2024, all UW faculty, staff and other academic personnel who are traveling overseas on official UW business will now be covered by an international emergency medical and security insurance policy. This coverage is provided at no cost to the traveler and differs from the current coverage in that it includes emergency medical benefits.
- The GME Office is supporting a new project called the Names & Pronunciations Initiative, which aims to not only highlight the importance of name pronunciations, but also improve communication by providing physical badges (for those who want one) which include users’ written phonetic name pronunciation. Anyone interested in learning more about the project or who wants to order a pronunciation badge can do so here: https://www.names-pronunciations-initiative.com/. If you receive a badge for someone not in your program or if you have any questions, please email the project lead, Sudiptho (UW MS4) at sudiptho@uw.edu.
People
- A team at UW Medicine has created the Multidisciplinary Thoracic Aortic Program (MTAP) to provide holistic, team-based care for complex aortic disease. With a team of cardiologists, cardiac surgeons, clinic staff, genetic counselors, medical geneticists and vascular surgeons, the MTAP team discusses 250 to 300 patient cases annually. Team members from the Department of Medicine include Catherine Otto (professor), Yonatan Buber (Adult Congenital Heart Disease Associate Program Director), James Kirkpatrick (Advanced Cardiac Imaging Program Director), and Peter Byers (professor). Read the full story from The Huddle.
- Justin Bullock, fellow, Nephrology, is senior author of “The Next Era of Assessment: Can Ensuring High-Quality, Equitable Patient Care Be the Defining Characteristic?” in Academic Medicine.
- Sarah Gunby, fellow, is lead author, and Lisa Strate, professor, Gastroenterology, is senior author of “Smoking and alcohol consumption and risk of incident diverticulitis in women” in Clinical Gastroenterology and Hepatology.
- Vishesh Kapur, Sleep Medicine Program Director, is quoted in “No more ‘spring forward’ if new bill passes WA state legislature” from KIRO.
- Leo Morales, Assistant Dean for Healthcare Equity and Quality, is quoted in “What Recovery?” in Palabra. He is also quoted in “Long COVID’s deep impact on Latinos” from The Oregonian.
- Emily Myers, Developmental-Behavioral Pediatrics Program Director, is quoted in “Screen time for kids under 2 linked to sensory differences in toddlerhood” from ABC News.
- Sarah Prager, Complex Family Planning Program Director, is quoted in “Umbilical Cord Blood Transplant Saved Woman From Rare Cancer” from The Huddle.
- Namrata Singh, Rheumatology Associate Program Director, is lead author of “Frailty and risk of serious infections in patients with rheumatoid arthritis treated with biologic or targeted-synthetic DMARDs” in Arthritis Care & Research. She is also quoted in “Frailty Worsens Side Effects of Rheumatoid Arthritis Treatment” in MedPage Today.
- Crystal Brown, assistant professor, Pulmonary, Critical Care and Sleep Medicine, is lead author and Bessie Young, Vice Dean of Equity, Diversity, and Inclusion, is senior author of “Discriminatory healthcare experiences and medical mistrust in patients with serious illness” in the Journal of Pain and Symptom Management. Department of Medicine co-author is Kristine Cueva.
- Sharing news about our trainees: two of UW Medicine’s Top 10 Huddle Stories of 2023 were about trainees (Get to Know Our Chief Residents and Fellows & Volunteer-Led Virtual Bedside Concert Program Thrives)!
- Check out the Otolaryngology Head and Neck – Winter 2023 Newsletter for trainee features and faculty highlights.
by amande | Jan 5, 2024 | Announcements, News

Byron Joyner, MD, MPA
The Names & Pronunciations Initiative (NPI) is a community project that aims to help people pronounce each other’s names correctly. All of us are many things. But our names define us. As our community becomes more diverse, NPI will help us correctly pronounce others’ names. NPI does this very simply: it makes physical pronunciation tags that can be layered behind our hospital ID badges.
In partnership with the Office of Healthcare Equity – and many other UW Medicine groups, I am proud to support this project as it helps us to get to know each other better. This month I have invited the NPI project lead, UW 4th year UWSOM medical student Sudiptho (suh-dip-doe) Paul, to share NPIs’ origins. It is my hope that NPI will help everyone feel welcome in our community.
Byron Joyner, MD, MPA
Vice Dean for Graduate Medical Education, Designated Institutional Official

Sudiptho Paul, MS4
The inspiration behind the Names & Pronunciations Initiative (NPI) stems from a personal journey marked by an awareness of the impact that mispronunciations can have on one’s sense of self and belonging. Having navigated predominantly white spaces in my youth, college, and work as a first-generation Bangladeshi-Thai American, I experienced firsthand both the subtle and significantly negative impacts of name mispronunciations on my educational and professional development and well-being—an “othering” experience common to many people.
This awareness continued during virtual medical school amid the challenges of the COVID-19 pandemic when particularly distressing mispronunciations of my name drove me to address the issue more proactively. Having successfully advocated for the integration of NameCoach—a program facilitating audio recordings of name pronunciations—into the medical school’s online systems, it became apparent during my clinical rotations that something more tangible was needed for the face-to-face clinical settings.
Hence, I started NPI, which involved the creation of physical name pronunciation tags as a simple communication aid. Designed to layer behind UW hospital ID badges, these tags function as a helpful tool to facilitate more accurate name pronunciations in-person. NPI empowers individuals to cultivate stronger interpersonal relationships for communication and collaboration in our community— connections start with our names.
![Example of Names & Pronunciation Initiative Badge. Learn more about the project online [QR Code]. My name is pronounced:](https://sites.uw.edu/uwgme/files/2024/01/Badge-Example-25ed619a14af647a-150x150.jpeg) Implementing NPI required perseverance and teamwork to translate awareness into action. Despite facing initial setbacks in grant applications, the project eventually secured support through the 2023 UW Resilience & Compassion Seed Grant. The setting was ripe for collaboration, as I came to learn that other students, residents, fellows, attendings, and staff had also had similar conversations about the importance of correct name pronunciations. Coming together, we designed the tags, developed strategies for their distribution across the Washington, Wyoming, Alaska, Montana, Idaho (WWAMI) region, and engaged with various UW Medicine affiliated groups to foster the project’s success in our community. I also built NPI’s website, which serves as an information hub where people can order pronunciation tags and find other resources. Beyond improving name pronunciations, I want these tags to also prompt us all to reflect more about our names’ role on our identities. Who named you and why? How does it feel when it is pronounced correctly versus incorrectly? What does your name mean to you and what does it represent?
Implementing NPI required perseverance and teamwork to translate awareness into action. Despite facing initial setbacks in grant applications, the project eventually secured support through the 2023 UW Resilience & Compassion Seed Grant. The setting was ripe for collaboration, as I came to learn that other students, residents, fellows, attendings, and staff had also had similar conversations about the importance of correct name pronunciations. Coming together, we designed the tags, developed strategies for their distribution across the Washington, Wyoming, Alaska, Montana, Idaho (WWAMI) region, and engaged with various UW Medicine affiliated groups to foster the project’s success in our community. I also built NPI’s website, which serves as an information hub where people can order pronunciation tags and find other resources. Beyond improving name pronunciations, I want these tags to also prompt us all to reflect more about our names’ role on our identities. Who named you and why? How does it feel when it is pronounced correctly versus incorrectly? What does your name mean to you and what does it represent?
NPI can be regarded as a grassroots initiative driven by our community’s collective commitment to inclusivity. I hope this project’s manifestation inspires others to act on other issues, regardless of how minor a problem may seem—it is about encouraging small steps that contribute to a larger improvement in culture within UW Medicine and beyond.
Sudiptho Paul
4th Year Medical Student
University of Washington School of Medicine
by amande | Dec 21, 2023 | Announcements, Events, GME News & Notes, News
Dear GME Community,

Cindy Hamra Associate Dean, GME
December News & Notes has several useful reminders including information about accessing UW Medicine Care for Employees, accepting gifts from patients, and several great events in the new year.
From the GME Office, we’re excited to celebrate Dr. Itay Bentov, Associate Professor, Anesthesiology and Pain Medicine, as winner of the 2023 Bruce C. Gilliland Award. We also congratulate Dr. Tim Dellit on his appointment as CEO of UW Medicine and Dean of the School of Medicine. Dr. Dellit did his fellowship here at UWSOM in infectious diseases!
Dr. Joyner’s December blog shares our reflections on 2023. Happy holidays to those in our community who celebrate and wishing all a happy and healthy 2024!
Thank you,
Cindy
Policies and Processes
- The holiday season is often a time of giving by grateful patients, vendors, and other outside organizations. State employees within UW Medicine are governed by the Washington State Ethics in Public Service Act with regard to the gifts they may accept and how they may redirect gifts they cannot accept. Common questions about gifts from patients and other external sources (including food and beverages) and other related topics are answered in the Gifts from External Sources FAQs on the UW Medicine Compliance website. Additional information is available on the Internal Audit website.
- A reminder that residents and fellows are considered essential personnel who are expected to report for duty; please see guidance from Residency and Fellowship Position Appointment (RFPA) Agreement 2023-2024 and Executive Order 27: Suspended Operations Policy.
- Remember that trainees who are members of the RFPU-NW are entitled to one (1) paid personal holiday per calendar year. If unused in the calendar year, the personal holiday is forfeit, and it is not paid at separation. It is the employee’s responsibility to schedule the personal holiday before December 31st. If before the end of the calendar year the employee requests the use of their personal holiday in accordance with the employer’s time off or leave procedures and the employer denies the request, the employee is entitled to carry over the personal holiday to the next calendar year. Please see complete information in Article 12 of the RFPU-NW Contract.
- Welcome New Program Administrators:
- Sydney Anderson, Child Abuse Pediatrics
- The GME Appointment Manager position is now live, and we are accepting applications! You can find the position posted here. Hayley Fisher is happy to answer questions about the position.
- The ACGME has a weekly e-Communication. If you wish to receive it, email ACGMECommunications@acgme.org.
Events of Interest
- GME Lunch & Learns
- December 21: Canceled
- January 18: ACGME Surveys
- February 15: Washington Physicians Health Program (WPHP)
- Presentations from the November and December Program Administrator meetings are available on the Program Administrator Meetings page.
- We invite you to two evenings of writing and storytelling supported by the UW Medicine Well-Being Grant. Professor Susan Meyer at Seattle University will guide us to reflect on our personal and professional experiences from the pandemic into the present. You are welcome to join one or both of these free sessions (January 16th and February 6th).
- Navigating Parental Leave for Resident & Fellow Physicians will be Tuesday, February 6th from 6:30-7:30pm via Zoom. Please see the agenda. Register today. Registration closes February 2. If you can’t make it, a recording will be posted to the Housestaff Events webpage.
- Please join us on Tuesday, February 6, 2024, from 8:30am-12pm for the AY25 Onboarding Kickoff Meeting. This virtual event will provide an overview of the onboarding and reappointment processes for the upcoming academic year. Attendance at this meeting is highly encouraged for all program administrators and any department staff involved in the appointment and onboarding process of new residents and fellows, including those of you who are not program administrators but have roles in Workday. Please see the Save the Date email sent on December 21st for more information.
- Registration for the ACGME Meaning in Medicine 2024 Annual Education Conference is open! The conference is scheduled to take place in Orlando, Florida at the Rosen Shingle Creek Resort March 7-9, 2024. More information can be found on the conference website. Support for meeting attendance is ensured by the clinical chair in every new Program Director Appointment Letter.
- The University of Washington School of Medicine is sponsoring the 2024 Graduate Medical Education (GME) Summit. The focus will be collaborating to address workforce needs within the WWAMI region and beyond. Early bird registration for the GME Summit 2024 is now open! Join us on April 25-26, 2024, in Anchorage, Alaska at the BP Energy Center. Stay tuned in the coming months as we announce speakers.
- Please save the date(s)! The GME Office is pleased to invite program leadership (PDs, APDs, PAs) to participate in an educational series that we will be offering throughout 2024. We have designed this series in response to cross-program challenges as observed in our ACGME surveys and in our work supporting programs and trainees. See 11/9 email from Cindy Hamra for more information.
- Other GME Events can be found on our calendar.
Projects and Resources
 Please review the GME Annual Program Timeline for important dates for the months of December and January including: Milestones mid-year reporting, semi-annual Procedures Certification entry in MedHub, ACGME Annual Survey preparation, and SF Match registration (for applicable programs).
Please review the GME Annual Program Timeline for important dates for the months of December and January including: Milestones mid-year reporting, semi-annual Procedures Certification entry in MedHub, ACGME Annual Survey preparation, and SF Match registration (for applicable programs).- Our PLAs team is hoping to make strides in communication and improving the process for our community in several ways:
- We created a new, simplified introduction video for the PLA process as a whole here.
- We want to make sure the barriers to completing a rotation request or PLA are as low as possible. If you could please fill out the linked survey and provide feedback it would be helpful and allow us to improve the process.
- Please review the email from Chris Gibson sent on 12/19 for data on expiring PLAs.
- Please review “Access to UW Medicine Care for Employees” from The Huddle for information about help for UW Medicine employees and their families to gain better access to UW Medicine facilities and providers.
- The WWAMI Institute for Simulation in Healthcare (WISH) is the simulation-based education program serving all of UW Medicine, since 2005. WISH is undergoing some exciting developments and is seeking input from all users (as well as would-be future users) to help inform strategic plans for the next 5 years. By the end of this year, please take a few moments to provide your responses around both current and anticipated future simulation-based utilization, and services that would benefit your training programs in the coming years. For additional comments or questions, please reach out to WISH Associate Director, Megan Sherman or Chief of the Division for Healthcare Simulation Science, Dr. Rob Sweet.
- Every year, the UW School of Medicine Alumni Association recognizes exceptional alumni with a series of awards. We encourage UW School of Medicine alumni, faculty, staff and other professional colleagues to nominate alumni for one or more of our awards. All alumni who received a degree from, or completed residency or fellowship training in, a program administered by the UW School of Medicine or one of our academic departments are eligible. Visit the website for full descriptions of the Distinguished Alumni Award, the Alumni Humanitarian Award, the Alumni Service Award and the Alumni Early Achievement Award. Nominations for the 2024 awards are open; you may submit nominations until December 31, 2023 here.
- The UW Office of Global Affairs is excited to announce that effective January 1, 2024, all UW faculty, staff and other academic personnel who are traveling overseas on official UW business will now be covered by an international emergency medical and security insurance policy. This coverage is provided at no cost to the traveler and differs from the current coverage in that it includes emergency medical benefits.
- The GME Office is supporting a new project called the Names & Pronunciations Initiative, which aims to not only highlight the importance of name pronunciations, but also improve communication by providing physical badges (for those who want one) which include users’ written phonetic name pronunciation. Anyone interested in learning more about the project or who wants to order a pronunciation badge can do so at: https://www.names-pronunciations-initiative.com/. If you receive a badge for someone not in your program or if you have any questions, please email the project lead, Sudiptho (UW MS4).
- The GME Office has posted an updated letter from Dr. Joyner for prospective residents and fellows to our GME Prospective Residents & Fellows page.
People
- Justin Bullock, fellow, Nephrology, is co-author of “Stereotype Threat and Gender Bias in Internal Medicine Residency: It is Still Hard to be in Charge” in the Journal of General Internal Medicine.
- Anne Browning, UW Assistant Dean of Well-Being, shares some lessons from rowing on how to cultivate resilience in your own life in “What the 1936 UW Rowing Team Teaches Us About Resilience” from The Huddle.
- In the latest resident scholarship spotlight, “Medical Mistrust Among Black Patients with Serious Illness,” Kristine Cueva designed and led a mixed methods study to better understand patient perspectives. View spotlight.
- In recognition of their substantial contributions to local healthcare quality and safety, Gwen Bernacki, clinical assistant professor (Cardiology), Medhavi Bole, clinical assistant professor (Allergy and Infectious Diseases), Jurjen de Jong, Internal Medicine chief resident, Soloman Graf, associate professor (Hematology and Oncology), and Sarah Sanghavi, clinical associate professor (Nephrology) have been awarded the title of Practitioner Lead in Quality & Safety (PLQS) within the Hospital & Specialty Medicine service line at the VA Puget Sound Health Care System.
- Congratulations to Ksenia Ershova, resident, Anesthesiology & Pain Medicine, and Bonica Scholar, for winning the 2023 FAER Resident Scholar Abstract Award at the 2023 ASA meeting.
- The Society of General Internal Medicine is honoring members at the front lines of Social Justice with their member highlight series, “Frontliners: Social Justice.” Rebecca Gold, resident, Internal Medicine, is highlighted this month. She recently presented a poster in collaboration with UW’s Breast Health Equity group on the inequities of breast cancer care along racial lines, particularly for Somali and Ethiopian immigrants living in Seattle. Read the challenges in conducting her research and how she hopes this research will help address inequities in breast cancer care in the future.
- Mark Harrast, Sports Medicine PM&R Program Director, is featured in “Ways to stop muscle cramps from interrupting your run, by Dr. Mark Harrast, medical director of the UW Medicine Seattle Marathon,” “ Mark Harrast demystifies the pre-race meal,” and “Dr. Mark Harrast shares advice about how to manage a pesky hamstring injury” from Right as Rain.
- Nicholas Johnson, Critical Care Medicine Associate Program Director, is co-author of “Vaccine Effectiveness Against Influenza A-Associated Hospitalization, Organ Failure, and Death: United States, 2022-2023” in Clinical Infectious Diseases.
- Department of Medicine Chair Barbara Jung is PI on a new grant from the Department of Defense for her project “Mechanisms of Activin Signaling in Acute Pancreatitis” to test the hypothesis that activin A signaling is an early and targetable component of morbidity/mortality-inducing inflammatory response in severe acute pancreatitis (AP).
- Vishesh Kapur, Sleep Medicine Program Director, is quoted in “UW sleep expert among those pushing federal leaders for permanent standard time” from KIRO News.
- Several Department of Medicine researchers have received additional funding from the Breast Cancer Research Foundation (BCRF) to continue ongoing studies. Among them is who will continue to investigate whether a progesterone tracer known as FFNP-PET can be used as a better predictive marker of endocrine therapy’s efficacy. Read the full story from Hutch News.
- Pediatric Allergy & Immunology fellow Gabriel Mendoza has been appointed to the ACGME Review Committee for Allergy and Immunology.
- Neha Deshpande, Lisa Chew, Jill Watanabe and Somnath Mookherjee (Academic Hospitalist Fellowship Program Director) wrote “A letter to today’s academic generalist mentor” and Jennifer Wright, Helen Starks, Lauren Beste, Jared Klein (Addiction Medicine Associate Program Director) and Somnath Mookherjee wrote “Lessons from a project-based mentorship initiative” in SGIM Forum.
- Leo Morales, Assistant Dean for Healthcare Equity and Quality, is featured in “Washington lacks Spanish-speaking nurses — for an Everett student, it’s personal” from Herald Net. He is also co-author of “Critical Reflections on This Historical Moment for Community-engaged and Participatory Research” in Progress in Community Health Partnerships: Research, Education, and Action.
- Sarah Prager, Complex Family Planning Program Director, is featured in “How the overturn of ‘Roe’ still impacts Washington abortion care” from Crosscut.
- Russ Van Gelder, chair of Department of Ophthalmology, is featured in “Sleep experts, physicians address effects of increased travel on student-athletes, offer recommendations” from UW News.
-
by amande | Dec 8, 2023 | Announcements, News
-
 Byron Joyner, MD, MPA |
 Jennifer Best, MD |
 Cindy Hamra JD, MA |
It is startling that we are facing the end of another calendar year, yet here it is: December! What a year! Through our windows, the Seattle afternoons are dark, but in our hearts, there is light, especially as we reflect on what our community has accomplished in 2023.
Over the past year, the GME Office has developed and shared a new strategic plan that will guide our focus over the next six years. We are particularly proud of this ambitious plan which represents input from a broad range of community members. Movement on this plan will bring material improvements to all elements of our already-outstanding learning environment, which we have intentionally centered on advocacy for our trainees. In the New Year, we welcome involvement from community members who are particularly interested in one or more of our initiatives.
The GME team continues to evolve. This year, we said hello to team members Chris Gibson (Affiliations and Agreements Specialist), Ivy Gibson (eLearning Experience Developer), Bethany Griffitts (Fiscal Specialist), Allison Shults (RMS and Information Systems Manager) and Amy Wheat (Wellness Counselor). The team supported the rollout of six new GME programs (Advanced Cardiac Surgery, Colon and Rectal Surgery, FM Medical Student Education, Global and Rural Health, Pediatric Neuro-Oncology), including the first rural residency in internal medicine in the United States – the University of Washington Alaska Internal Medicine Rural Residency Program. And we are excited to welcome the inaugural cohort for the new LEAD-UP leadership program – a partnership between UW GME and the Office of Healthcare Equity (OHCE).
Seattle had the privilege this year of playing host in November to the American Association of Medical Colleges’ (AAMC) Learn Serve Lead Annual Conference, in the brand new and stunning Seattle Convention Center – Summit location. It was wonderful to see so many UW SOM educators representing our School of Medicine and presenting there, and to celebrate the 75th anniversary of the WWAMI program with our new Dean, Dr. Tim Dellit who welcomed more than 100 people at the UW Welcome Event.
The work of GME is dynamic, rich, and essential for the health of our community. This is true regardless of where and how that work is accomplished: at the bedside, in conference rooms, in administrative offices, operating rooms, clinics, or on-line. It simply would not be possible without each of you who has joined us on this collective journey. We look forward to more opportunities in 2024 to come together again in person and to celebrate the shared goals that unite our individual efforts as a beautiful whole.
Our best to each of you this season and Happy New Year!
Byron Joyner, MD, MPA
Vice Dean for GME and DIO
Jennifer Best, MD
Associate Dean, Accreditation and Education
Cindy Hamra, JD
Associate Dean, Operations and Administration
by amande | Nov 17, 2023 | Announcements, Events, GME News & Notes, News

Dear GME Community,

Cindy Hamra Associate Dean, GME
I’m pleased to share several great educational events and opportunities in the November News & Notes, including the excellent Optimizing MedHub Lunch & Learn, 2024 ACGME conference registration, a new 2024 GME educational series and the November PA meeting recording.
This article from the UW Medicine Newsroom focuses on practice in rural areas: Docs trained in rural areas tend to practice in rural areas. Our Department of Family Medicine has a Chelan Rural Training Program that is designed to train physicians for rural practice.
November is Native American Heritage Month! This article in The Huddle has information about the history, cultures and achievements of Native American communities, including articles about Northwest Native Art and Native American contributions to public health as well as a guide to events and heritage sites in Seattle.
Finally, sending off Khrystine Buccat, our amazing GME Appointment Manager, as she transitions to the Department of Obstetrics & Gynecology as the new Maternal-Fetal Medicine Division Administrator. Khrystine’s last day in GME is November 22. We wish her all the best and will be posting the opening shortly!
Thank you,
Cindy

Policies and Processes
- COVID Vaccination are Required for All Current and Future Trainees at Seattle Children’s – Due by 12/11/2023. All residents, fellows, and medical students rotating or have access to Seattle Children’s after 12/11/2023 are required to have full COVID vaccination, including the new 2023-2024 Monovalent COVID-19 mRNA Vaccine, or have request ed an exception prior to working at Seattle Children’s. The sponsoring program/institution will be responsible for ensuring trainee compliance. For more information, trainees should go to CHILD (Seattle Children’s intranet).
- The holiday season is often a time of giving by grateful patients, vendors, and other outside organizations. State employees within UW Medicine are governed by the Washington State Ethics in Public Service Act with regard to the gifts they may accept and how they may redirect gifts they cannot accept. Common questions about gifts from patients and other external sources (including food and beverages) and other related topics are answered in the Gifts from External Sources FAQs on the UW Medicine Compliance website. Additional information is available on the Internal Audit website.
- Explore benefits options at UW Benefits & Resource Fairs (including virtual option)
Learn about your benefits options in advance of open enrollment (November 1 – December 15) at one of the UW onsite benefits fairs, or an ongoing virtual fair.
- A reminder that residents and fellows are considered essential personnel who are expected to report for duty; please see guidance from Residency and Fellowship Position Appointment (RFPA) Agreement 2023-2024 and Executive Order 27: Suspended Operations Policy.
- Remember that trainees who are members of the RFPU-NW are entitled to one (1) paid personal holiday per calendar year. If unused in the calendar year, the personal holiday is forfeit, and it is not paid at separation. It is the employee’s responsibility to schedule the personal holiday before December 31st. If before the end of the calendar year the employee requests the use of their personal holiday in accordance with the employer’s time off or leave procedures and the employer denies the request, the employee is entitled to carry over the personal holiday to the next calendar year. Please see complete information in Article 12 of the RFPU-NW Contract.
- Welcome New Program Administrators:
- Ruby Tang, Obstetric Anesthesiology, Liver Transplant Anesthesiology, Regional Anesthesiology
- Serena Wong, Neuromuscular Medicine, Vascular Neurology
- The GMEC has approved appointment of the following new program directors; ACGME appointments require Review Committee (RC) confirmation:
- Chris Burke, Cardiothoracic Surgery and Thoracic Surgery – Integrated (Interim)
- Paige Keasler, Obstetric Anesthesiology
- Matthew Phelps, Breast Imaging (non-ACGME)
- Porshia Underwood, Obstetrics and Gynecology
- The ACGME has a weekly e-Communication. If you wish to receive it, email ACGMECommunications@acgme.org.
Events of Interest
- GME Lunch & Learns
- November 16: Optimizing MedHub Settings, slides and recording now available
- December 21: Canceled
- January 18: ACGME Surveys
- Registration for the ACGME Meaning in Medicine 2024 Annual Education Conference is open! The conference is scheduled to take place in Orlando, Florida at the Rosen Shingle Creek Resort March 7-9, 2024. More information can be found on the conference website. Support for meeting attendance is ensured by the clinical chair in every new Program Director Appointment Letter.
- Please save the date(s)! The GME Office is pleased to invite program leadership (PDs, APDs, PAs) to participate in an educational series that we will be offering throughout 2024. We have designed this series in response to cross-program challenges as observed in our ACGME surveys and in our work supporting programs and trainees. See 11/9 email from Cindy Hamra for more information.
- The University of Washington School of Medicine is sponsoring the 2024 Graduate Medical Education (GME) Summit. Please Save the Date to join us on April 25-26, 2024, in Anchorage, Alaska. Registration will open in December.
- Other GME Events can be found on our calendar.
Projects and Resources
 Please review the GME Annual Program Timeline for important dates for the months of November and December including: NRMP Match deadlines, fall Milestones reporting, semi-annual Procedures Certification entry in MedHub, ERAS preseason setup (Dec Cycle), and AAMC/GME Track GME Census deadlines.
Please review the GME Annual Program Timeline for important dates for the months of November and December including: NRMP Match deadlines, fall Milestones reporting, semi-annual Procedures Certification entry in MedHub, ERAS preseason setup (Dec Cycle), and AAMC/GME Track GME Census deadlines.- Presentation from Nov 14 Program Administrator meeting is now available on the Program Administrator Meetings page.
- The GME Office is supporting a new project called the Names & Pronunciations Initiative, which aims to not only highlight the importance of name pronunciations, but also improve communication by providing physical badges (for those who want one) which include users’ written phonetic name pronunciation. Anyone interested in learning more about the project or who wants to order a pronunciation badge can do so at: https://www.names-pronunciations-initiative.com/. If you receive a badge for someone not in your program or if you have any questions, please email the project lead, Sudiptho (UW MS4).
- The WWAMI Institute for Simulation in Healthcare (WISH) is the simulation-based education program serving all of UW Medicine, since 2005. WISH is undergoing some exciting developments and is seeking input from all users (as well as would-be future users) to help inform strategic plans for the next 5 years. By Friday, December 15th, please take a few moments to provide your responses around both current and anticipated future simulation-based utilization, and services that would benefit your training programs in the coming years. For additional comments or questions, please reach out to WISH Associate Director, Megan Sherman or Chief of the Division for Healthcare Simulation Science, Dr. Rob Sweet.
- Every year, the UW School of Medicine Alumni Association recognizes exceptional alumni with a series of awards. We encourage UW School of Medicine alumni, faculty, staff and other professional colleagues to nominate alumni for one or more of our awards. All alumni who received a degree from, or completed residency or fellowship training in, a program administered by the UW School of Medicine or one of our academic departments are eligible. Visit the website for full descriptions of the Distinguished Alumni Award, the Alumni Humanitarian Award, the Alumni Service Award and the Alumni Early Achievement Award. Nominations for the 2024 awards are open; you may submit nominations until December 31, 2023 here.
- The GME Office has posted an updated letter from Dr. Joyner for prospective residents and fellows to our GME Prospective Residents & Fellows page.
- Based on feedback from our community, in AY23 the GME Office developed Total Compensation sample statements for trainees at the R1 and R4 levels, meant to reflect incoming residents and incoming fellows, respectively. The R1 & R4 Total Compensation sample statements have been updated for AY24. These resources are posted to the GME Prospective Residents and Fellows page under Compensation.
- The Leave of Absence webpage contains LOA planning information and resources along with an intake form to contact GME for leave planning assistance: Leave Planning Submission Form.
People
- Ryan Abe, Internal Medicine Health Equity Pathway Director, is senior author of “Equity M&M — Adaptation of the Morbidity and Mortality Conference to Analyze and Confront Structural Inequity in Internal Medicine” in the Journal of General Internal Medicine. Department of Medicine co-authors are Hannah Oren and Helen Jack.
- Christopher Alawode, OEM resident, is featured in “How occupational medicine physicians support workers” from the Environmental & Occupational Health Sciences website.
- Joey Chiang, resident, Internal Medicine, is co-author of “Homelessness and Incidence and Causes of Sudden Death: Data From the POST SCD Study” in JAMA Internal Medicine.
- John Choe, Internal Medicine Residency Associate Program Director, is featured in the latest faculty spotlight from the Department of Medicine. Read his faculty spotlight on their news site.
- A cornerstone of the VA’s efforts to strengthen and diversify the VA scientific work force, the Summer Research Program offers research experiences to Veterans, children of Veterans, and underrepresented students. The 3-year pilot program started in June 2022 at 21 VA sites across the country. Co-directed by Lindsey Anderson, acting assistant professor, and Jose Garcia, Geriatric Medicine Research Pathway Program Director, the Seattle site primarily provides students with experience in research related to age/cancer-related declines in muscle mass and function (human, animal, and benchwork) and traumatic brain injury (TBI) related hormone dysfunction (human). Learn more on the Department of Medicine news site.
- Mark Harrast, Sports Medicine PM&R Program Director, is featured in “What Runners Need to Know About the Immune System” and “3 Simple Ways to Help Runner’s Knee” from Right as Rain.
- Carrie Ho, fellow, is lead author, and Stephen Smith, associate professor (Hematology and Oncology) is senior author of “Pembrolizumab with R-CHOP in Previously Untreated DLBCL: Sustained, High Efficacy and Safety with Long-Term Follow-Up” in Clinical Lymphoma, Myeloma & Leukemia. Department of Medicine co-authors are Ajay Gopal, Brian Till, Mazyar Shadman, Ryan Lynch, Andrew Cowan, Heather Rasmussen, Chaitra Ujjani and Ryan Cassaday.
- Vishesh Kapur, Sleep Medicine Program Director, is featured in “UW sleep expert among those pushing federal leaders for permanent standard time” from Kiro 7.
- Ayesha Khader, resident, Internal Medicine is lead author and Pavan Bhatraju, associate professor (Pulmonary, Critical Care and Sleep Medicine) is senior author of “The Interaction of Acute Kidney Injury with Resuscitation Strategy in Sepsis: A Secondary Analysis of a Multicenter, Phase 3, Randomized Trial (CLOVERS)” in the American Journal of Respiratory and Critical Care Medicine. Department of Medicine co-authors are Leila Zelnick, Neha Sathe, Bryan Kestenbaum, Jonathan Himmelfarb, and Nicholas Johnson
- Emily Liang, fellow, is lead author, and Jordan Gauthier, associate professor (Hematology and Oncology) is senior author of “Factors associated with long-term outcomes of CD19 CAR T-cell therapy for relapsed/refractory CLL” in Blood Advances. Department of Medicine co-authors are Aya Albittar, Jennifer Huang, Alexandre Hirayama, Erik Kimble, Andrew Portuguese, Aude Chapuis, Mazyar Shadman, Brian Till, Ryan Cassaday, Filippo Milano, Hans-Peter Kiem, Stanley Riddell, Cameron Turtle and David Maloney.
- Leo Morales, Assistant Dean for Healthcare Equity and Quality, is this year’s recipient of the Secretary’s Award from the Washington state Department of Health. The Award recognizes the strong work occurring around Washington state in the field of public health and links that work with the dedicated people working every single day to protect and promote the health and well-being of everyday Washingtonians. Dr. Morales was honored for his work protecting and promoting the health of Latino communities in Washington state and across the Pacific Northwest. Learn more on the Department of Medicine news site.
- Sarah Prager, Program Director, Complex Family Planning, is featured in “How Telemedicine Makes Abortion More Accessible” from The Huddle.
- Ganesh Raghu, Interstitial Lung Disease Program Director, is senior author of “Idiopathic pulmonary fibrosis: aligning murine models to clinical trials in humans” in the Lancet Respiratory Medicine.
- May Reed, Geriatric Medicine Associate Program Director, is PI for the TRIAD study within the Dog Aging Project. TRIAD (Test of Rapamycin in Aging Dogs) is a clinical trial currently underway across the United States that seeks to assess the effects of rapamycin on health and aging in dogs. Learn more about the project.
- Ginny Ryan, Reproductive, Endocrinology and Infertility Program Director, is featured in “Updated ‘infertility’ definition could help more hopeful LGBTQ+ parents in Washington” from Axios Seattle.
- Laura Quinnan, Medical Director for the UWMC – Northwest Campus, received the Hospitalist of the Year award at the recent American College of Physicians Washington state chapter meeting.
by amande | Nov 9, 2023 | Announcements, News

Byron Joyner, MD, MPA
Many members of our community are familiar with the GME Wellness Service, a vital part of the GME Team. Our four amazing counselors provide tremendous support for our residents and fellows. This month, Dipti Chrastka, Director of the GME Wellness Service, shares an update about the robust services that create a healthier learning environment for our trainees.
Byron Joyner, MD, MPA
Vice Dean for Graduate Medical Education, Designated Institutional Official
Our health and well-being have taken a toll over the last few years: the COVID-19 pandemic, which resulted in social isolation; racial unrest: and the more recent news of war and violence in Ukraine and the Middle East. We may experience feelings of fear, uncertainty, sadness, stress, and overall distress.
This season of shorter, cooler, darker days with less day light can also adversely impact our mood, sleep cycles, sap our energy and daily functioning.
Many of our medical professionals may face many stressors that affect their mental and physical health.
Resident and fellow well-being is a priority for UW GME which has been providing care to our community for over two decades.
Our GME Wellness Team provides a wide spectrum of services to build connection and foster a culture of holistic wellness. The GME Wellness team members are all licensed and skilled clinicians who bring their unique experiences in working with health care professionals.
Some of the many ways the Wellness Service supports you:
- Counseling support: Our services are free, unlimited, and completely confidential. We offer daytime, as well as evening wellness appointments to accommodate our trainees’ busy schedules. We are currently offering virtual sessions, which reduces barriers, and takes away the stress of commuting, parking, and finding time in your already packed day to get support.
In AY23, we supported 249 unique residents, fellows, and partners/spouses with a total of 1,734 visits. We provided individual counseling, couples counseling, and connected many trainees with referrals to in-house specialists (e.g., a psychiatric provider and learning specialist).
- We are proud to share that most of our clients are self-referred and many suggest our services to their colleagues.
- In July 2023, we were very proud to be able to expand our wellness services to non-ACGME We currently serve nearly 1660 residents and fellows as well as their partners and spouses.
- Facilitating presentations and group conferences: We partner with programs to understand the needs of our residents and fellows, facilitate discussion groups, share wellness tips and resources. In AY23, we presented to 12 programs and groups.
- Consultation and Advocacy: Our discussions with individuals and programs help us have a deeper understanding of trends and issues in the larger system so we can advocate for improvements. We brainstorm and dialogue with GME and UW Medicine leadership to provide our residents and fellows avenues to raise concerns. Some examples include: identifying quiet spaces at our hospital sites; reporting microaggressions in a group; advocating for lightboxes in closed, windowless spaces within our hospitals to combat Seasonal Affective Disorder (SAD); and generally enhancing well-being around our campuses.
- Community building: We host events for residents and fellows to meet and build social connections which allow networking to enhance well-being. We also publish a monthly newsletter, the Wellness Corner, to share local events, resources, and spotlight Wellness Wonders in our community.
Your input is vital to our success. Qualitative and quantitative data helps us evaluate our impact and make programmatic modifications.
Here’s some valuable feedback we received from our community in July.
- “You value prioritizing mental health, wellness in residency training and our Wellness Services.”
- “Having an unbiased, non-judgmental human being to provide longitudinal support, resources: someone who understands the stresses of residency and fellowship is a strength of our wellness service.”
- “Emphasis on accessibility, removing barriers and offering evening hours for Wellness sessions.”
Connection is key and one antidote to isolation. The Wellness Team is honored to serve you and look forward to connecting with you. To read more about our service, visit our webpage. Visit our scheduling page to schedule a wellness appointment or establish care.
Reach out to us – seeking support is an act of courage! We are here to share in your joys, lighten your burdens, and celebrate you as we build a healthier community together.

GME Wellness Counselors
by amande | Oct 20, 2023 | Announcements, Events, GME News & Notes, News

Dear GME Community,

Cindy Hamra Associate Dean, GME
I’m writing to share the October News & Notes.
As October ends, programs are busy with recruitment activities, and I want to give kudos to the Network of Underrepresented Residents & Fellows (NURF), which hosted the fourth annual diversity town hall. Dr. Ivonne Beltran Lara, president of NURF, also authored the October DIO Blog. A reminder to programs of GME’s Recruitment Resources page as well. GME has created a new Welcome Video, which is posted to our Prospective Residents & Fellows page. Thanks to our extremely talented Lead eLearning User Experience Designer, Joe Wilson!
Yesterday, the GME Lunch & Learn highlighted safety and support resources for trainees. The recording is posted to our L&L page, and I wanted to remind you of our Workplace Health & Safety page as well as Information by Training Site. Please also remember that concerns can be reported to GME via the Report a Concern form.
Local and international news are difficult to watch right now, and the days are getting shorter. Many members of our community are affected by these challenging events, and I encourage you to offer compassion and support. Our wonderful GME Wellness counselors are available to support residents and fellows and OFA has a robust list of UW Supports and Mental Health Resources.
Thank you,
Cindy
Policies and Processes
- Please see the information from UW Medicine Employee Health and Infection Prevention & Control Teams on ‘When Will Masking in Clinical Spaces Be Required?’
- Remember that trainees who are members of the RFPU-NW are entitled to one (1) paid personal holiday per calendar year. If unused in the calendar year, the personal holiday is forfeit, and it is not paid at separation. It is the employee’s responsibility to schedule the personal holiday before December 31st. If before the end of the calendar year the employee requests the use of their personal holiday in accordance with the employer’s time off or leave procedures and the employer denies the request, the employee is entitled to carry over the personal holiday to the next calendar year. Please see complete information in Article 12 of the RFPU-NW Contract.
- Explore benefits options at UW Benefits & Resource Fairs
Learn about your benefits options in advance of open enrollment (November 1 – December 15) at one of the UW onsite benefits fairs, or an ongoing virtual fair.
- A reminder that residents and fellows are considered essential personnel who are expected to report for duty; please see guidance from Residency and Fellowship Position Appointment (RFPA) Agreement 2023-2024 and Executive Order 27: Suspended Operations Policy.
- Welcome New Program Administrators:
- Esben Kincaid, Family Medicine Sports Medicine and Global Health
- Tony Trejo, Clinical Neurophysiology, Epilepsy, Neurocritical Care, Neuromuscular Medicine, and Vascular Neurology
- The GMEC has approved appointment of the following new program directors; ACGME appointments require Review Committee (RC) confirmation:
- Sarah Wahlster, Neurocritical Care fellowship program (ACGME application pending)
- Elizabeth Harrington, Obstetrics and Gynecology Global and Rural Health fellowship (non-ACGME)
- The ACGME has a weekly e-Communication. If you wish to receive it, email ACGMECommunications@acgme.org.
Events of Interest
- GME Lunch & Learns
- October 19: Resident/Fellow Safety and Support Resources; slides and recording now available
- November 16: Optimizing MedHub Guidance for Programs!
- Family Building During Residency & Fellowship Monday, October 30th from 6-7:45pm PST. Dr. Rachel Whynott, a reproductive endocrinologist, and infertility specialist, will answer questions and educate trainees about defining future family goals, how fertility changes with age, and options for delaying fertility and/or addressing infertility. Dr. Whynott may also be joined by a physician panel representing diverse families. Register today. Registration will close on October 26th.
- Please save the date for the 2024 University of Washington Center for Surgical Ethics Seminar! This will be held hybrid & in-person on Thursday and Friday, August 1st and 2nd 2024. Details of the event are still being finalized, but please stay tuned for more information! In the meantime, check out our Surgical Ethics Website.
- Other GME Events can be found on our calendar.
Projects and Resources
 Please review the GME Annual Program Timeline for important dates for the months of October and November, including: October eLearning launch deadline, NRMP Match deadlines, fall Milestones reporting, ERAS preseason setup (Dec Cycle).
Please review the GME Annual Program Timeline for important dates for the months of October and November, including: October eLearning launch deadline, NRMP Match deadlines, fall Milestones reporting, ERAS preseason setup (Dec Cycle).- New SafeCampus videos aim to foster resilient, inclusive spaces: Two new videos for faculty, supervisors and managers were created to promote a safe, equitable workplace culture by teaching evidence-based prevention principles that address identity-based conflicts and build skills within the UW community.
- The GME Office has an open recruitment for a second Float Administrator on our team (see posting, req. 210821). In addition to ensuring continuity of key operations of ACGME and non-ACGME programs residency and clinical fellowship programs during periods of program administrator transition or leave, the Float Administrator also works on special projects in the GME Office with the operations/administration and accreditation teams.
- Trainees are encouraged to subscribe to UW Medicine STAT|INFO ADVISORY which has been designed to disseminate official information via text message to keep the UW Medicine workforce informed during emergencies and situations that might disrupt normal operations. See flyer for complete information and consider sharing.
- UW Medicine launched the Bias Reporting Tool in early 2021 to provide our community with a new way to report incidents of bias. Since then, over 1,000 events have been reported. The Second Annual Community Report provides information about 372 events reported in the past year for the purpose of raising awareness about what our community is experiencing. This information helps us see patterns of biased behavior and identify areas needing more investment, training, policy, practice and process changes.
- Every year, the UW School of Medicine Alumni Association recognizes exceptional alumni with a series of awards. We encourage UW School of Medicine alumni, faculty, staff and other professional colleagues to nominate alumni for one or more of our awards. All alumni who received a degree from, or completed residency or fellowship training in, a program administered by the UW School of Medicine or one of our academic departments are eligible. Visit the website for full descriptions of the Distinguished Alumni Award, the Alumni Humanitarian Award, the Alumni Service Award and the Alumni Early Achievement Award. Nominations for the 2024 awards are open; you may submit nominations until December 31, 2023 here.
- Have questions about managing your schedule in MedHub? Don’t forget about the resources and recordings available on our GME MedHub website.
- The UWMC Department of Public Safety is happy to announce the highly anticipated bike cage on the Northwest campus is ready for use. This secured bicycle storage area is located on the 1st floor, Southeast corner of the parking garage. The bike locker is complete with racks and simple tools for most of your bicycle needs. To have access to this bike locker added to your Husky Card, please email either Joshua Kinman at jkinman9@uw.edu or Deborah Wheat at dwheat3@uw.edu.
- The GME Office has posted an updated letter from Dr. Joyner for prospective residents and fellows to our GME Prospective Residents & Fellows
- Based on feedback from our community, in AY23 the GME Office developed Total Compensation sample statements for trainees at the R1 and R4 levels, meant to reflect incoming residents and incoming fellows, respectively. The R1 & R4 Total Compensation sample statements have been updated for AY24. These resources are posted to the GME Prospective Residents and Fellows page under Compensation.
- Our new Leave of Absence webpage is now live on the GME website. Here you will find LOA planning information and resources along with an intake form to contact GME for leave planning assistance: Leave Planning Submission Form. This form can be completed by trainees or program leadership. The December 2022 Lunch & Learn on ‘Leave Policy and Guidelines’ provides an overview of both these new resources; please see the recording and slides.
People
- UW Medicine, University of Washington and Fred Hutchinson Cancer Center leaders have been highlighted among other “movers and shakers” in the Puget Sound Business Journal’s 2023 Power 100.The fifth annual list recognizes UW Medicine Interim CEO Tim Dellit, Harborview CEO Sommer Kleweno Walley, UW President Ana Mari Cauce and Fred Hutch President and Director Thomas Lynch for their contributions to our community. Read more in a recent article from The Huddle.
- The new Alaska Internal Medicine Rural Residency Program has released a fantastic recruitment video!.
- Jessica Barsano, Medical Genetics Resident, was nominated and selected to serve as the resident representative on the ACGME Review and Recognition Committee (RRC).
- Sayuli Bhide, Internal Medicine R3, received funding from the Rheumatology Research Foundation Resident Research Preceptorship to study “Sex differences in frailty and mortality in Veterans with Rheumatoid Arthritis.” She will be working on this proposal with Katie Wysham (Rheumatology) and Joshua Baker (UPenn).
- John Choe, Internal Medicine Associate Program Director, is senior author of “Evaluation of an Individualized Learning Plan Template for the Transition to Residency” in the Journal of Graduate Medical Education.
- Dipti Chrastka, Director of the GME Wellness Service, is quoted in Prioritizing Mental Health for Healthcare Workers in the UW Medicine Huddle.
- Başak Çoruh, Pulmonary and Critical Care Program Director, is the inaugural Medical Educator Scholar Diversity Fellowship Mentor for the Association of Pulmonary & Critical Care Medicine Program Directors (APCCMPD) and CHEST Medical Educator Scholar Diversity Fellowship Award. Established in 2023, the CHEST and APCCMPD Medical Educator Diversity Scholarship Fellowship Award recognizes the value of a diverse community in improving medical education in pulmonary and critical care medicine.
- Thomas Dodson, Chair of Oral and Maxillofacial Surgery in the School of Dentistry, is featured in UW scientists use stem cells to regenerate tooth enamel from KING 5.
- Richard Ellenbogen, Professor and Chair of Neurological Surgery and Program Director for the Neurosurgery Residency Program, was elected as Chair of the ACGME Neurological Surgery Review Committee.
- Barbara Goff, Professor and Chair of Obstetrics & Gynecology, was honored with the 2023 Dr. Saul E. Rivkin Award from the Rivkin Center. Her research interests include early detection of ovarian cancer, novel therapeutic drugs for ovarian and other gynecologic malignancies, and surgical training and education. She also helped develop the Ovarian Cancer Symptoms Questionnaire to help people experiencing key ovarian cancer symptoms communicate that information to their physician.
- Ganesh Raghu, Intersitial Lung Disease Program Director, is lead author of “Treatment of Systemic Sclerosis-associated Interstitial Lung Disease: Evidence-based Recommendations. An Official American Thoracic Society Clinical Practice Guideline” in the American Journal of Respiratory and Critical Care Medicine. Department of Medicine co-author is Gregory Gardner. Dr. Raghu is also co-author of “De novo design of highly selective miniprotein inhibitors of integrins αvβ6 and αvβ8” in Nature Communication.
- James Kirkpatrick, Advanced Cardiac Imaging Program Director, is co-author of “Expanding the Paradigm for Cardiovascular Palliative Care” in Circulation.
- Somnath Mookherjee, Academic Hospitalist Fellowship Program Director, is the new director of the Center for Learning and Innovation in Medicine Education (CLIME). The mission of CLIME is to create a diverse, inclusive, and welcoming community that works together to optimize teaching skills, foster educator career development, and support educational scholarship.
- Leo Morales, Assistant Dean for Healthcare Equity and Quality, is quoted in “COVID Tests Are Available to Anyone in the Country with a US Address, Regardless of Legal Status” in Latin Times. He is featured in “‘You’re my queen.’ A Latina wife with dementia and the loving husband who cares for her” from KUOW.
- The 2023 recipients and nominees for the Inaugural Department of Medicine Outstanding Staff Awards were recognized and celebrated at a recent ceremony. The Outstanding Staff Award recognizes and celebrates exceptional staff members who are dedicated to supporting our missions of teaching, healing, discovery, and diversity, and upholding core values. Shinetra Pryor (Program Operations Specialist for the Geriatrics and Palliative Care Fellowship Programs) was among the winners.
- Nahid Rashid, fellow, is lead author and Marco Mielcarek, professor (Hematology and Oncology) is senior author of “Impact of Donor Statin Treatment on Graft-versus-Host Disease after Allogeneic Hematopoietic Cell Transplantation” in Transplantation and Cellular Therapy. Department of Medicine co-authors are Stephanie Lee, Paul Martin and Rainer Storb.
- Namrata Singh, Rheumatology Associate Program Director, has been selected to receive a 2023 UCLA MSTAR Best Research Mentor Award. MSTAR (Medical Student Training in Aging Research) is a combined program (UCLA, UCSF and UW) that provides medical students short-term research training in aging and geriatrics with successful mentors in the field, with the goal of encouraging medical students to consider careers as physician scientists in aging research.
- Alyssa Stephenson-Famy, Obstetrics and Gynecology Associate Program Director, is an author on “Does the Degree Matter? MD and DO Students Who Match Into OB/GYN Report Different Experiences in US Undergraduate Medical Education” from the Journal of Graduate Medical Education.
- Tracy Tylee, Metabolism, Endocrinology and Nutrition Program Director, is quoted in “Nonsurgical Option for More Large Thyroid Nodule Patients?” in Medscape.
- Andrew Wescott, fellow, Cardiology, is the recipient of a 2024 Postdoctoral Fellowship from the Washington Research Foundation. The foundation supports 12 postdocs annually from institutions across Washington state, with the goal to promote innovative discoveries and technologies that lead to the delivery of a new project, service or practice to the public. Dr. Wescott’s project is “Mechanisms of Arrhythmogenic Calcium Release in Cardiac Stem Cell Therapy.”
by amande | Oct 11, 2023 | Announcements, News

Byron Joyner, MD, MPA
The Network of Underrepresented Residents and Fellows (NURF) began its mission of community outreach, mentorship, recruitment and retention, 14 years ago. This diverse resident-run group has consistently been a safe harbor community for many of our residents and fellows. I am very proud to sponsor this group with Office of Healthcare Equity. This month I have invited Dr. Ivonne Beltran Lara to be the guest writer for the DIO blog.
Byron Joyner, MD, MPA
Vice Dean for Graduate Medical Education, Designated Institutional Official

Ivonne Beltran Lara, MD
When I was searching for a residency program, I was looking for a program supportive of individuals underrepresented in medicine and with diverse identities and backgrounds – an institution that fosters diversity and values the integrity of hard work, as well as healthcare equity and inclusion of those who are historically disenfranchised. In 2020, deciphering which institution truly upheld this mission was especially difficult as we were faced with Zoom screens and the lack of human connection. It was the first year that residency interviews went virtual, and applicants would have to rank a list of programs based only on virtual encounters.
Humanity was facing a worldwide pandemic that was wreaking havoc in all communities especially in Black, Indigenous, people of color (BIPOC) communities. The reality of the atrocious effects of inequities and structural racism in our society was on the forefront of every media outlet and in the conversations of everyone. This made it even more important for me to find a residency that would help me thrive and celebrate the various identities I hold: I am a woman, a person of color, a first-generation physician, an immigrant, and a Deferred Action for Childhood Arrivals (DACA) recipient. These identities made me the courageous and tenacious person I am today, and yet they are also vulnerabilities in environments where diversity, equity, and inclusion (DEI) efforts are not supported or celebrated.
During the process of my residency interviews, I was introduced to the Network of Underrepresented Residents and Fellows (NURF) at the University of Washington School of Medicine. Through NURF, I met residents and fellows who were part of the different training programs and who identified as underrepresented individuals in medicine (URiM).
I attended the first ever NURF Diversity Town Hall led by Drs. Ashley Eaves (Physical Medicine & Rehabilitation) and Joseph Nelson (Family Medicine), NURF’s 2020-2021 President and Vice President, respectively. I was impacted by the leaders who were at the forefront of DEI work and the community that it brought together. The community I met during this town hall surged my interest in UW. NURF would be the organization and platform through which I could continue DEI work. It would shepherd and strengthen a community I could depend on when presented with challenges that underrepresented physicians experience in a historically exclusionary field.
As a resident, I became an active participant in NURF. For the 2023-2024 academic year, I have the privilege of serving as president of NURF. Dr. Jessica Sher (Physical Medicine & Rehabilitation, VP of NURF) and I partnered to lead this year’s Diversity Town Hall. We were grateful to have the support of Graduate Medical Education (GME) and the Office of Healthcare Equity (OHCE) once again.
During our town hall, we presented our commitment to anti-racism, healthcare equity, and diversity efforts. We introduced NURF as a community for residency applicants who identify as underrepresented in medicine and their allies. Our purpose is to ensure applicants know that NURF is committed to supporting medical trainees who need a safe space and who are looking for a community they can count on. We are also committed to holding our faculty leaders and the institution accountable to the dire need to recruit and retain diverse trainees and faculty. My hope is that via this Diversity Town Hall, we reassure future URiM residents that we are a network committed to the efforts that allow underrepresented groups in medicine to thrive and will advocate for their success.
Thanks to those who continue their work to support NURF and make this town hall an annual reality. I am continuously proud and inspired by the work my colleagues and past NURF members do to make sure our community continues to be a palpable presence.
Ivonne Beltran Lara, MD
R3, Family Medicine
NURF President 2023-2024
The UW Medicine Huddle recently featured an article on NURF’s 2023 Diversity Town Hall: NURF Hosts Diversity Town Hall.
by amande | Sep 21, 2023 | Announcements, Events, GME News & Notes, News
Dear GME Community,

Cindy Hamra Associate Dean, GME
Sharing our September News & Notes with information about the LeadUp program and Gilliland Award (nominations for both closing soon), PDDS, the fertility benefits survey, the new bike cage at UWMC-NW and a host of other information and opportunities.
I also want to recognize that Hispanic and Latinx Heritage Month, which started on September 15, celebrates the history, diverse cultures, achievements and contributions of Hispanic Americans. September is also National Suicide Prevention Month, a chance to raise awareness of risk factors, provide help for those who may be struggling, and support those affected by the suicide of a loved one. Please see resources from Forefront Suicide Prevention at UW and a reminder that the GME Wellness Service offers free and confidential counseling for our trainees (including non-ACGME fellows).
Thanks,
Cindy

Policies and Processes
- Get Ready for Respiratory Virus Season: Masking and Vaccine Information
- UW Medicine plans to require universal masking in patient care areas during respiratory virus season based on metrics that are being developed with regional health systems.
- The Employee Health flu vaccine campaign will begin on Sept. 25.
- Employees should stay home when they have respiratory virus symptoms and also test for COVID-19. If you test positive, you should also complete the UW Medicine Employee Health COVID-19 Contact Tracing Survey. Once you report a positive test, you will immediately receive an email with details about isolation during your illness.
- For more information about the respiratory virus season, see COVID-19 and the flu this fall (with Dr. John Lynch).
- UWSOM has decided to continue to exclude the class rank/quartile ranking and summary word in the MSPE. Please see 8/25 email sent on behalf of Gabriel Sarah and the Office of Academic Affairs for more information.
- Effective July 1, 2023, the GME Meals Policy and SCH Meals Policy have been updated to reflect an increase in meal reimbursement prices.
- The GME Office and GME Wellness are pleased to announce that as of July 1, 2023, the GME Wellness Service will support our non-ACGME fellows without faculty titles or with an existing counseling relationship. For those non-ACGME fellows with faculty titles, there are a number of support resources available via UWSOM Faculty Affairs. Please direct any questions to GME Director of Wellness, Dipti Chrastka.
- Residents and fellows who wish to moonlight must renew existing outside work activity requests for AY24. All requests for outside work must be reapproved each academic year. Please review the GME Outside Work webpage for the Moonlighting and Outside Work Policy and Outside Work Request Forms. Please email Angela James with any questions.
- Individuals who would like to request a disability accommodation should reach out to the GME Office (Bre Smith) as soon as possible so that we can work with the Disability Services Office to support the program and trainee through the process.
- The UW Medicine Bias Reporting Tool is for sharing incidents of bias including racism, sexism, ableism, discrimination of any form or other behaviors that do not reflect the prioritization of inclusion and equity expected in all areas of our community. Please feel free to share this flyer and postcard within your programs and workspaces.
- The GME Concern Reporting tool is available to any members of the GME community to report concerns about the learning environment.
- Welcome New Program Administrators:
- Daniel Willems, Diagnostic Radiology
- The GMEC has approved appointment of the following new program directors; ACGME appointments require Review Committee (RC) confirmation:
- Matthew Kogut, Interventional Radiology Independent & Interventional Radiology Integrated
- Pamela Valentino, Pediatric Transplant Hepatology (interim)
- The ACGME has a weekly e-Communication. If you wish to receive it, email ACGMECommunications@acgme.org.
Events of Interest
- GME Lunch & Learns
- September 21: IMGs and Visa Sponsorship; slides and recording now available
- October 19: Resident/Fellow Safety and Support Resources
- Registration for our Fall Program Director Development Series on Wednesday, September 27 from 12:00 PM – 2:00PM (PST) is now open. Registration will close the evening of September 22. This season we are excited to invite Dr. Chrissy Babcock, Associate Dean and DIO for Graduate Medical Education, and Dr. Vineet Arora, Dean of Medical Education, join us from the University of Chicago, Pritzker School of Medicine to present on “Embedding Residents & Fellows into Institutional Learning Environment Initiatives.” Each program is required to have a PD or APD (or, if necessary, a member of the core faculty) attend these virtual events. We also welcome all other faculty and administrators seeking faculty development.
- Make sure to save the date for our Spring sessions on March 19 and April 8
- For a variety of upcoming events and resources, please see the NURF newsletter emailed out by Tammy Ramirez on September 13.
- GME Outreach Event for trainees at SCH on October 5 from 11am to 1 pm. We encourage trainees to stop by to say hello, meet our GME team members and take a packed lunch. Please look for an email closer to the event with specific room details.
- Other GME Events can be found on our calendar.
Projects and Resources
 Please review the GME Annual Program Timeline for important dates for the months of September and October, including: Annual Program Evaluation deadline, AAMC/GME Track National GME Census, ERAS opening (Sept Cycle), NRMP and SF Match timelines, and October eLearning launch.
Please review the GME Annual Program Timeline for important dates for the months of September and October, including: Annual Program Evaluation deadline, AAMC/GME Track National GME Census, ERAS opening (Sept Cycle), NRMP and SF Match timelines, and October eLearning launch.- Have questions about managing your schedule in MedHub? Don’t forget about the resources and recordings available on our GME MedHub website.
- We are distributing a needs assessment survey to understand better UWSOM learners’ potential utilization of fertility benefits in light of proposed legislation that may impact such coverage. Please access the survey here: UW SOM Trainee Fertility Survey. The survey will remain open through October 1, 2023.
- The GME Office is accepting nominations for the Bruce C. Gilliland Award for Excellence in Teaching of Residents and Fellows. The Gilliland Award is awarded annually to a faculty member who is actively engaged in clinical and didactic training or in the implementation of a graduate medical education curriculum. Candidates should have demonstrated excellence in teaching over time and must have served for at least three years within UW Medicine or an affiliated training site as a teacher of residents and/or fellows. The Nomination deadline has been extended to Sept. 29.
- Faculty, residents and fellows who use Epic at UW Medicine are strongly encouraged to complete the UW Medicine Epic EHR Satisfaction survey and provide feedback on the Epic application. If you are a clinician that uses Epic regularly, please take 10-12 minutes to provide your feedback on the Epic application by end of day Monday, Sept. 25. To begin the survey, please visit uwehrsurvey.com. You will be asked to enter your name and email to ensure survey responses are valid. At the end of the survey, you can choose to allow your identity to be connected to your responses, which will enable UW Medicine IT Services to link your survey to your actual Epic usage data. Your responses will be kept strictly confidential. While participation is voluntary, your insights and candid feedback on the efficiency of the Epic application, quality of Epic training, and how Epic use is impacting your daily work/life balance will play a pivotal role in shaping the future improvements to our EHR system.
- Last October, the GME Office launched a Post-Recruitment Survey for residency and fellowship programs to send to interviewed applicants. The Survey was designed to be followed longitudinally over subsequent recruitments cycles. As a reminder, we ask programs to include the following message in post-recruitment survey communications to interviewed applicants: The Graduate Medical Education Office at the University of Washington School of Medicine is conducting a survey of residency and fellowship applicants interviewed during the current recruitment season to assess factors that contributed to ranking decisions. Results of the survey will help improve the quality of our learning environment. Please take 1-2 minutes to complete this brief and anonymous survey – https://forms.microsoft.com/r/9WhQckPbZb.
- The UWMC Department of Public Safety is happy to announce the highly anticipated bike cage on the Northwest campus is ready for use. This secured bicycle storage area is located on the 1st floor, Southeast corner of the parking garage. The bike locker is complete with racks and simple tools for most of your bicycle needs. To have access to this bike locker added to your Husky Card, please email either Joshua Kinman at jkinman9@uw.edu or Deborah Wheat at dwheat3@uw.edu.
- The GME Office is proud to partner with the Office of Healthcare Equity to sponsor Leadership Education to Advance Diversity among Underrepresented Populations in Medicine (LEAD-UP). Applications are due 9/27. Please see 8/24 email from Dr. Joyner for more information.
- Every year, the UW School of Medicine Alumni Association recognizes exceptional alumni with a series of awards. We encourage UW School of Medicine alumni, faculty, staff and other professional colleagues to nominate alumni for one or more of our awards. All alumni who received a degree from, or completed residency or fellowship training in, a program administered by the UW School of Medicine or one of our academic departments are eligible. Visit the website for full descriptions of the Distinguished Alumni Award, the Alumni Humanitarian Award, the Alumni Service Award and the Alumni Early Achievement Award. Nominations for the 2024 awards are open; you may submit nominations until December 31, 2023 here.
- UW Medicine Announces Results from Equity, Diversity & Inclusion (EDI) Survey are available.
- The GME Office has posted an updated letter from Dr. Joyner for prospective residents and fellows to our GME Prospective Residents & Fellows
- Based on feedback from our community, in AY23 the GME Office developed Total Compensation sample statements for trainees at the R1 and R4 levels, meant to reflect incoming residents and incoming fellows, respectively. The R1 & R4 Total Compensation sample statements have been updated for AY24. These resources are posted to the GME Prospective Residents and Fellows page under Compensation.
- Trainees are encouraged to subscribe to UW Medicine STAT|INFO ADVISORY which has been designed to disseminate official information via text message to keep the UW Medicine workforce informed during emergencies and situations that might disrupt normal operations.
- Our new Leave of Absence webpage is now live on the GME website. Here you will find LOA planning information and resources along with an intake form to contact GME for leave planning assistance: Leave Planning Submission Form. This form can be completed by trainees or program leadership. The December 2022 Lunch & Learn on ‘Leave Policy and Guidelines’ provides an overview of both these new resources; please see the recording and slides.
People
- Sally Baker, fellow, Allergy and Infectious Disease, is quoted in “Seal bit swimmer through wetsuit in Washington. Then she needed special medicine” in the Bellingham Herald.
- Katherine Bennett, Geriatric Medicine Program Director, and May Reed, Geriatric Medicine Associate Program Director, are featured in “Two Geriatricians Give 6 Tips for Healthy Aging” from The Huddle.
- Debra Cherry, Occupational and Environmental Medicine Program Director, provides tips for teens and their families on navigating workplace safety issues in Teen Workers ‘Need to Know They Have Rights’ from the UW Newsroom.
- John Choe, Internal Medicine Associate Program Director, is senior author of “Exploring Competency-Based Medical Education Through the Lens of the UME-GME Transition: A Qualitative Study” in Academic Medicine.
- Christopher Sanford, Global Health Program Director, is quoted in “Vaccinating people from airplanes is not feasible, contrary to Instagram post” from US Today.
- The Department of Surgery Newsletter ‘Surgery Synopsis’ features many voices of the GME community, including Program Directors, trainees, and program staff. Check out the Summer 2023 issue.
- Ian Maloney, Anesthesiology Resident, is featured in “What Our Patients are Saying” with the following quote, “Special shout out to Dr. Ian Maloney! He was the kindest, warmest, most wonderful member of the team that I met that day. His demeanor and presence made me feel so at ease… He’s the kind of person that ABSOLUTELY should be in healthcare.”
- May Reed, Geriatric Medicine Associate Program Director, is quoted in “The Future of Human Longevity” in Health News.
- Ginny Ryan, Reproductive Endocrinology and Infertility Program Director, is quoted in “Congress makes fresh push to cover fertility treatments for military veterans” from Axios.
- Doug Wood, Department of Surgery Chair, is featured in “How To Catch Lung Cancer Early and Why It’s Important” from Right as Rain by UW Medicine.
by amande | Sep 8, 2023 | Announcements, News

Byron Joyner, MD, MPA
Lead donation from Drs. Paul and Bonnie Ramsey fuels excellence in GME Program and healthcare equity across WWAMI region
We are thrilled to share some incredible news that exemplifies the spirit of generosity and dedication to UW Medicine’s mission to improve the health of the public: a $10,000 personal donation from Drs. Paul and Bonnie Ramsey to the Vision Fund for Graduate Medical Education (GME), matched by a $10,000 grant from the Josiah Macy Jr. Foundation, where Dr. Paul Ramsey is a Trustee Emeritus.
The Vision Fund for GME is an endowed fund at the University of Washington that will distribute annual funding for use across the five-state WWAMI region to advance the programs’ diversity, equity and inclusion programs and related efforts. The mission of the Josiah Macy Jr. Foundation is to improve health by advancing the education and training of health professionals.
Drs. Paul and Bonnie Ramsey, exemplary healthcare leaders in our community for over 30 years, firmly believe that excellence in the Graduate Medical Education (GME) program is paramount for our institution to progress towards its mission of improving health outcomes for all people. Their vision for the future of medicine has inspired countless physicians, researchers and healthcare professionals throughout their careers, and we are deeply grateful for their commitment and support.
These new funds, combined with gifts from dozens of alumni and friends who have supported the Vision Fund for GME since its inception in 2019, ensure that our GME program will be bolstered, creating a profound ripple effect that will positively impact residency and trainee education. By investing in our trainees’ growth and nurturing the next generation of medical professionals, we can cultivate healthier communities across our region.
Now, we extend an invitation to all members of our community to join in this transformative endeavor. Your contribution, no matter the size, will make a meaningful difference in shaping the future of the University of Washington’s GME programs and improving public health across the WWAMI region. Together, we can strengthen our commitment to excellence and inclusivity, fostering a healthier world for all.
I invite you to join me in making a donation to the Vision Fund for GME online here, or connect with the UW Medicine Advancement Office directly at writemed@uw.edu or 206.543.5686.
Thank you for your continued support and belief in our shared mission to improve the health of the public.
With gratitude,
Byron Joyner, MD, MPA
Vice Dean for GME and DIO
by amande | Aug 28, 2023 | Announcements, Events, GME News & Notes, News
Dear GME Community,

Cindy Hamra Associate Dean, GME
Last Friday 8/18 was GME Professional’s Day and we gathered most of the GME team for an end of season event – it was a great time to be together and strengthen our team, and also to celebrate the UWSOM GME Professionals who support trainees, programs and departments in this crucial part of our mission.
If you haven’t yet seen President Cauce’s blog post regarding the Supreme Court’s decision on affirmative action in university admissions, it’s posted here: Affirmative action ruling won’t change our values or our mission. A reminder to our programs of the recruitment Town Halls 8/30 and 8/31, which is an opportunity to ask questions and discuss the impact(s) of this decision.
August News and Notes has information about the UWSOM MSPE, LEAD-UP, GME Recruitment Town Halls and lots of other interesting and valuable events.
Thanks,
Cindy
Policies and Processes
- UWSOM has decided to continue to exclude the class rank/quartile ranking and summary word in the MSPE. Please see 8/25 email sent on behalf of Gabriel Sarah and the Office of Academic Affairs for more information.
- As many programs starting recruitment and application reviews, we want to share some reminders about acceptable license examinations.
- Under the GME Licensure Examination Policy, residents and fellows must pass one of the following examinations for licensure:
- United States Medical Licensing Examination (USMLE)
- Comprehensive Osteopathic Medical Licensing Examination (COMLEX)
- Medical Council of Canada Qualifying Examination (MCCQE)
- Each year we receive questions from programs about whether the USMLE is also required for applicants who completed either the MCCQE or COMLEX. The MCCQE is accepted for state licensure. Canadian medical school graduates who have completed the MCCQE do not also require the USMLE (exception for Canadians seeking sponsorship on an H-1B, which requires USMLE Step 3). The COMLEX is required for graduates of osteopathic medical schools. Applicants who have completed the COMLEX do not also require the USMLE.
- The GMEC approved revisions to the following policies at the August meeting. All are posted on the Policies and Procedures page of the GME website.
- Immunization and Health Screening Policy
- Effective July 1, 2023, the GME Meals Policy and SCH Meals Policy have been updated to reflect an increase in meal reimbursement prices.
- Based on feedback from residents and fellows that late and/or conflicting information about grant funding availability and impacts has caused confusion and frustration, the GME Office has developed a new Grant Funding Policy. We welcome your questions.
- The GME Office and GME Wellness are pleased to announce that as of July 1, 2023, the GME Wellness Service will be available to our non-ACGME fellows for those without faculty titles or with an existing counseling relationship. For those non-ACGME fellows with faculty titles (appointed as Acting Instructors), there are a number of support resources available via UWSOM Faculty Affairs. Please direct any questions to GME Director of Wellness, Dipti Chrastka.
- Residents and fellows who wish to moonlight must renew existing outside work activity requests for AY24. All requests for outside work must be reapproved each academic year. Please review the GME Outside Work webpage for the Moonlighting and Outside Work Policy and Outside Work Request Forms. Please email Angela James with any questions.
- Individuals who would like to request a disability accommodation should reach out to the GME Office (Bre Smith) as soon as possible so that we can work with the Disability Services Office to support the program and trainee through the process.
- The UW Medicine Bias Reporting Tool is for sharing incidents of bias including racism, sexism, ableism, discrimination of any form or other behaviors that do not reflect the prioritization of inclusion and equity expected in all areas of our community. Please feel free to share this flyer and postcard within your programs and workspaces.
- The GME Concern Reporting tool is available to any members of the GME community to report concerns about the learning environment.
- Welcome New Program Administrators:
- Michelene Nguyen, Pediatric Infectious Diseases
- Krista Wintrode, Occupational and Environmental Medicine
- The GMEC has approved appointment of the following new program directors; ACGME appointments require Review Committee (RC) confirmation:
- Hamid Chalian, Thoracic Imaging (Interim)
- Douglas Franzen, Emergency Medicine (Interim)
- Joshua Fischer, Family Medicine Seattle & Family Medicine Chelan
- Margaret Hsu, Pain Medicine
- Sarah Menashe, Pediatric Radiology
- The ACGME has a weekly e-Communication. If you wish to receive it, email ACGMECommunications@acgme.org.
Events of Interest
- GME Lunch & Learns
- July 20: ADS Annual Update + Program Oversight; recording and slides available
- August 17: Canceled
- September 21: IMGs and Visa Sponsorship
- GME Recruitment Town Halls: please join us for a GME Town Hall on one of the dates/times below. Registration is required so we can approximate the number of participants and collect your questions in advance. Zoom links for the webinars will be sent to you upon registration.
- Register for August 30 at 7am
- Register for August 31 at 6pm
- Panelists: Dr. Byron Joyner, Vice Dean and DIO, GME; Dr. Suzanne Allen, Vice Dean for Academic, Rural and Regional Affairs; Paula Houston, Chief Equity Officer, and David Kerwin, Division Chief, Office of the Attorney General of Washington.
- GME Outreach Event for trainees at UWMC-ML on August 31 from 11am to 1 pm. Please stop by to say hello, meet our GME team members and take a packed lunch. Look for an email closer to the event with specific room details.
- Annual Life After Residency & Fellowship Seminar on Saturday, September 16: At this event we will share strategies, valuable insights and advice to support your transition into independent practice. Topics include avoiding job search pitfalls, how to negotiate, what to look for before you sign a contact and a panel of physicians from a variety of career tracks. The event will run via Zoom from 9am – 12:00pm. Attendance at this event is mandatory for some programs and others will block time for you to attend. Please check with your PA for details. Please mark your calendar – Register now. The event will be recorded and posted for streaming after the event.
- Other GME Events can be found on our calendar.
Projects and Resources
 The GME Office is proud to partner with the Office of Healthcare Equity to sponsor Leadership Education to Advance Diversity among Underrepresented Populations in Medicine (LEAD-UP). Applications are due 9/27. Please see 8/24 email from Dr. Joyner for more information.
The GME Office is proud to partner with the Office of Healthcare Equity to sponsor Leadership Education to Advance Diversity among Underrepresented Populations in Medicine (LEAD-UP). Applications are due 9/27. Please see 8/24 email from Dr. Joyner for more information.- The GME Annual Program Timeline: Please review for important dates for August and September.
- UW Medicine Announces Results from Equity, Diversity & Inclusion (EDI) Survey are available.
- The Macy Foundation is accepting applications for the Catalyst Awards. Six projects will be selected to receive up to $50K each over a 12-month period. Applications are due September 15!
- The GME Office is accepting nominations for the Bruce C. Gilliland Award for Excellence in Teaching of Residents and Fellows. The Gilliland Award is awarded annually to a faculty member who is actively engaged in clinical and didactic training or in the implementation of a graduate medical education curriculum. Candidates should have demonstrated excellence in teaching over time and must have served for at least three years within UW Medicine or an affiliated training site as a teacher of residents and/or fellows. Nominations are due September 8.
- The GME Office has posted an updated letter from Dr. Joyner for prospective residents and fellows to our GME Prospective Residents & Fellows page.
- As of July, UW employees will have access to a new benefit with the Washington State Employee Assistance Program (WA EAP)—a free health and well-being program that is just for Washington state employees. The WA EAP replaces CareLink.
- Based on feedback from our community, in AY23 the GME Office developed Total Compensation sample statements for trainees at the R1 and R4 levels, meant to reflect incoming residents and incoming fellows, respectively. The R1 & R4 Total Compensation sample statements have been updated for AY24. These resources are posted to the GME Prospective Residents and Fellows page under Compensation.
- Residents & Fellows – We want to hear from you! We hope to learn more about your current engagement with the UW GME Community and to understand opportunities for further connection and communication among trainees. Please take a moment to complete this survey and share your ideas about current and future GME education and community engagement events and tools.
- Residents and fellows are eligible to apply for a Housestaff Emergency Loan through the GME Office. The purpose of the loan fund is to provide emergency financial assistance to residents and fellows. The total amount of this loan has been increased from $1000 to $2500. Please see the loan form for complete details.
- Trainees are encouraged to subscribe to UW Medicine STAT|INFO ADVISORY which has been designed to disseminate official information via text message to keep the UW Medicine workforce informed during emergencies and situations that might disrupt normal operations.
- A new opt-in module, Prioritizing Ourselves When Fatigued is a 5 minute training intended as a brief reminder on the important issue of fatigue. Learning Gateway is happy to answer any questions about the module.
- Our new Leave of Absence webpage is now live on the GME website. Here you will find LOA planning information and resources along with an intake form to contact GME for leave planning assistance: Leave Planning Submission Form. This form can be completed by trainees or program leadership. The December 2022 Lunch & Learn on ‘Leave Policy and Guidelines’ provides an overview of both these new resources; please see the recording and slides.
People
- Christopher Blosser, Transplant Nephrology Associate Program Director, is quoted in “Cancer & organ transplant clinic” from WGEM.
- Markus Boos, Dermatology Program Director, is featured in Q&A: Pediatric dermatologist discusses impacts of climate change on patients from the UW Newsroom.
- Kelley Branch, Cardiovascular Disease Associate Program Director, is lead author and Nick Johnson, Critical Care Medicine Associate Program Director, is senior author of “Head-to-Pelvis CT Imaging after Sudden Cardiac Arrest: Current Status and Future Directions” in Resuscitation. Department of Medicine co-author is Peter Kudenchuk. Dr. Branch is also co-author of “Scientific document development standards for the society of cardiovascular computed tomography (SCCT): A statement from the SCCT Guidelines Committee” in the Journal of Cardiovascular Computed Tomography.
- Justin Bullock, fellow, Nephrology, is lead author of “‘Yourself in all your forms’: A grounded theory exploration of identity safety in medical students” in Medical Education. He is also co-author of “The Problem and Power of Professionalism: A Critical Analysis of Medical Students’ and Residents’ Perspectives and Experiences of Professionalism” and “From Eggshells to Action: A Qualitative Study of Faculty Experience Responding to Microaggressions Targeting Medical Students” in Academic Medicine.
- In the latest Thrivecast, “Transitioning from Trainee to Faculty,” Hugo Carmona, assistant professor, Pulmonary, Critical Care and Sleep Medicine, shares learnings and strategies in his own transition from fellow to faculty at UW. Hosted by Trish Kritek, Thrivecast provides tips to help clinicians, educators, and researchers thrive professionally in their careers, covering topics from time management and organization to leadership and self-advocacy.
- Başak Çoruh, Pulmonary and Critical Care Medicine Program Director, Amy Morris, and James Town were recognized by the American College of Chest Physicians (CHEST) as 2023 Distinguished CHEST Educators. This designation provides national-level recognition of excellence in continuing medical education through their commitment, involvement, and leadership in CHEST education programs and activities. CHEST is the global leader in advancing best patient outcomes through innovative chest medicine education, clinical research, and team-based care.
- Nicholas Johnson, Critical Care Medicine Associate Program Director, is co-author of “Total and Subgenomic RNA Viral Load in Patients Infected With SARS-CoV-2 Alpha, Delta, and Omicron Variants” in the Journal of Infectious Diseases.
- Department of Medicine Chair, Barbara Jung and her husband, Assistant Dean, Gerald Tolbert, have established the Barbara Jung and Gerald Tolbert – AGA Equity Focused Future Leaders Program Scholarship. This scholarship will support four scholarships for the Future Leaders Program for individuals from underrepresented backgrounds that are American Gastroenterological Association (AGA) Future Leaders or those that come from institutions that cannot support participation of an emerging leader into the AGA Future Leaders Program. The scholarship will start in 2024 and run for 20 years.
- Barbara Jung, professor and Department of Medicine Chair, wrote “Prior authorization, by any other name, threatens Washingtonians’ health” in The Olympian.
- Vishesh Kapur, Sleep Medicine Program Director, is quoted in “Jet Lag: Get Back in the Rhythm” in the New York Times.
- Natasha Kwendakwema, fellow, Hematology and Oncology, talked to OncLive about the “Effects of Financial Toxicity on Treatment Costs in Patients With Cancer.”
- Earlier this year, Blaine Menon and Kara Fitzgerald, Interventional Radiology Integrated Residents, had the unique opportunity to travel to Tanzania with Road2IR. Blaine participated in the department’s Global Health elective, and Kara joined him for a week as a volunteer. UW Radiology IR Program and Associate Program Directors, Jeff Chick and Matthew Abad-Santos also volunteered with them. Read about their experience in “Radiology Doctors Volunteer For Global Health Experience In Tanzania.”
- Adlai Grayson, Interventional Radiology resident, is featured in In their own words: Radiology physician advances diversity, equity and inclusion goals at conference.
- Hannah Linden, Hematology and Oncology Associate Program Director, discusses “FES PET for ER-Positive Breast Cancer: How Can It Help?” in Medscape. She also joined the Susan Komen Real Pink podcast to discuss “Understanding the Role of Diagnostic Imaging in Breast Care.”
- The Department of Otolaryngology Summer Newsletter features the work of trainees, Program Directors, and other department leaders.
- Shinetra Pryor, Geriatric Medicine and Palliative Medicine Program Administrator, received the inaugural Outstanding Staff Award from the Department of Medicine.
- Lucia Ramirez, Internal Medicine resident, is featured in this story in The Huddle.
- Bonnie Ronish, Occupational and Environmental Medicine Associate Program Director, is featured in “How ‘forever chemicals’ impact your health” from King 5 and in “How PFAS impact your health” in US Times Post. She is also featured in UW pulmonologist provides information on what smoke does to your body from KNDO and “Seattle air quality among worst in world due to wildfire smoke” from KIRO News.
- Dushyant Sahani, Department of Radiology Chair, is a recipient of the Radiological Society of North America (RSNA) Lifetime Honored Educator Award. This achievement recognizes his dedication to furthering the profession by delivering high-quality educational content.
- Namrata Singh, Rheumatology Associate Program Director, is lead author of “Immune-related adverse events after immune check point inhibitors: Understanding the intersection with autoimmunity” in Immunological Reviews and co-author of “Hydroxychloroquine use is associated with reduced mortality risk in older adults with rheumatoid arthritis” in Clinical Rheumatology.
- Joshua Thaler, Metabolism, Endocrinology and Nutrition Associate Program Director, is senior author of “Obesity-associated microglial inflammatory activation paradoxically improves glucose tolerance” in Cell Metabolism. Department of Medicine co-authors are Kelly Ness, Mauricio Dorfman, Jeremy Frey and Olivia Santiago. This article was featured as a Research Highlight in Nature Reviews Endocrinology.
- Bessie Young, Vice Dean for Diversity, Equity, and Inclusion, is the 2023 recipient of the Washington Physicians for Social Responsibility Paul Beeson Award. This award is given annually to an activist in the field of health care or health advocacy who has made a substantial contribution to peace, justice, and health in Washington state.
- Forbes ranked UW Medicine No. 14 in the nation in its annual ranking of America’s Best Employers for Women. They highlighted success in promoting women to top leadership positions across the organization and in providing other benefits such as childcare and eldercare services at a reduced cost.
- Congrats to the 17 trainee-led Wellbeing Grant winners! Please visit Well-Being Grants to see the list and descriptions of all funded grants for each entity.
by amande | Aug 18, 2023 | Announcements, News
The Association of Hospital Medical Education (AHME) has designated August 18, 2023 as GME Professionals Day.
GME Professionals Day is an opportunity for ACGME Sponsoring Institutions and Residency and Fellowship programs to celebrate the important contributions made by the GME professionals staffing their programs and central GME offices. As defined in the ACGME Common Program Requirements (CPRs), program administrators manage the day-to-day operations of the program and serve as an important liaison with learners, faculty, other staff members, as well as the ACGME. They serve as members of the leadership team, are critical to the success of the program, must possess skills in leadership and personnel management, and are expected to develop unique knowledge of the ACGME and Program Requirements, policies, and procedures. Sponsoring Institutions and programs are highly dependent on the knowledge, skills, and attitudes GME professionals possess and the dedication they exhibit in supporting the learning environment of the institution, their programs, and the success of their trainees.
And that’s just what the ACGME says.
We see you. We see your partnership with your faculty. We see you at educational sessions within our community – learning, growing, and challenging us with great questions. We hear your ideas. We know that you often serve as a safe and trusted confidante for residents and fellows and support them through the twists and turns of life and training. We see your commitment to planning events to bring people together to repair the disconnection of the pandemic years. We see your attention to deadlines and details, and there are oh-so-many of both in GME. And we know that your work may not be as visible or as visibly celebrated as that of the clinicians in your department.
We see you as experts. You are extraordinary. You truly make it all possible.
Today, we celebrate and thank each one of you. We look forward to being together in person this coming year.
The UW Graduate Medical Education Office Team
by amande | Aug 11, 2023 | Announcements, News
This month, we’re excited to share our new GME Strategic Plan. Work on this plan has been underway for over a year, and many members of our community have contributed, resulting in what we believe is a robust, trainee-focused, and comprehensive plan.
First, many thanks to our colleagues from across GME, the School of Medicine, and UW Medicine whose feedback and input helped shape this plan. On behalf of the GME Office, we’re excited to introduce our new Strategic Plan, for academic years 2024-29.
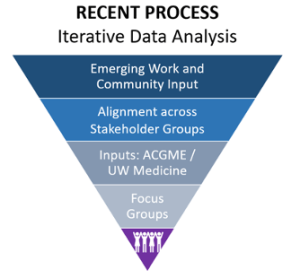 |
We have been working for over a year collecting input from our community, surveying our local and national landscape, vetting with our team, and requesting feedback from colleagues. This resulting GME Strategic Plan is intended to integrate with forthcoming UW School of Medicine and UW Medicine strategic plans, once finalized. |
| The overarching structure of the Plan is shaped by six Strategic Values: Advocacy, Communication, Expertise, Integration, People, and Quality & Value. These values shaped our AY 2020-23 Strategic Plan, and, because we believe so strongly that our values have not changed, we decided to keep them to guide our work. |
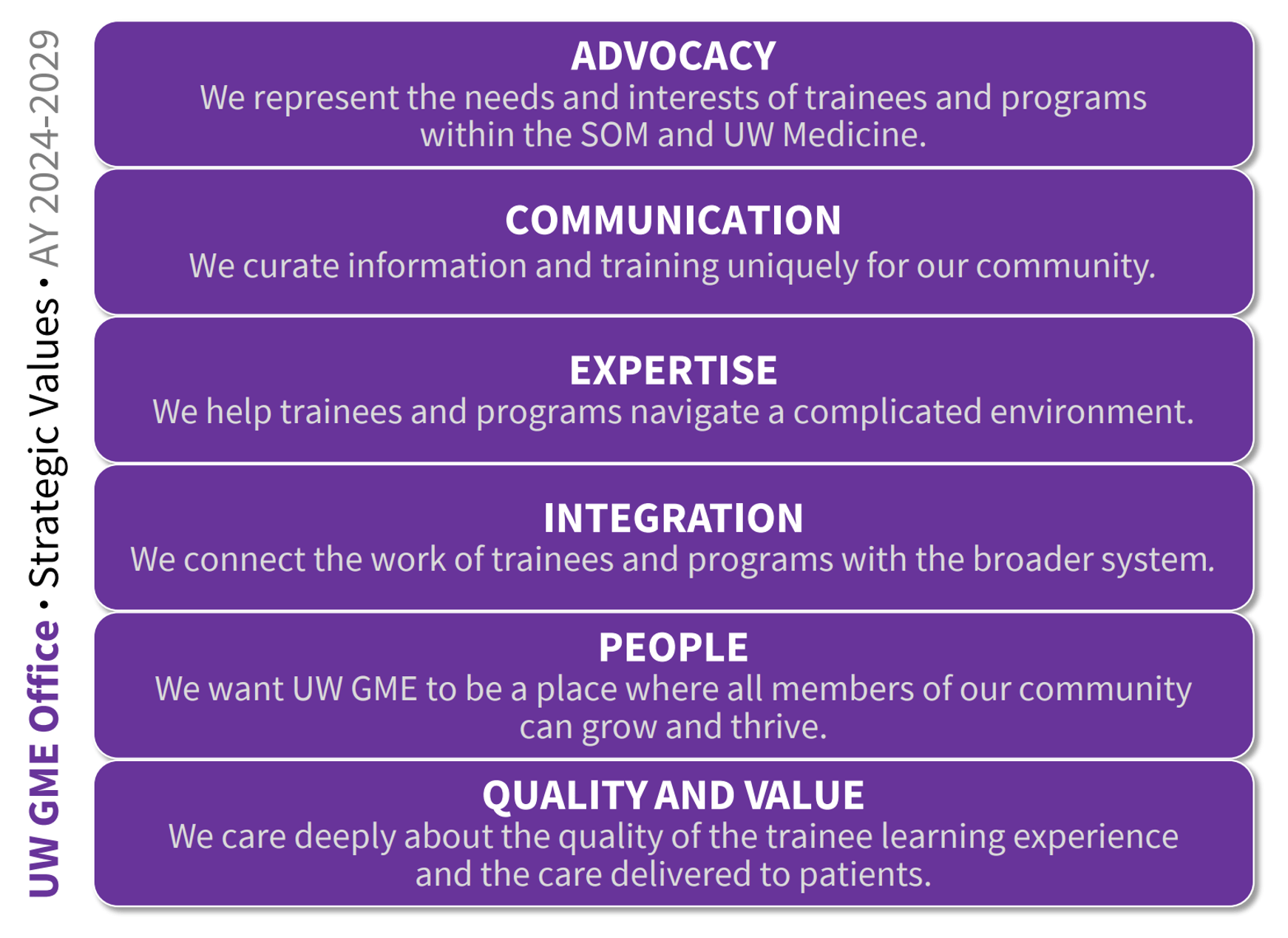 |
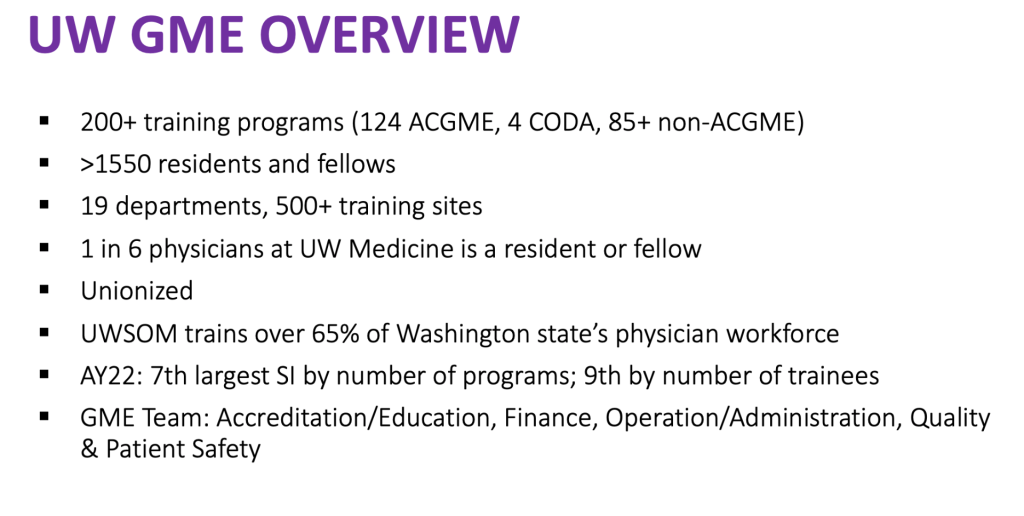 |
GME has a significant footprint in both the School of Medicine, and UW Medicine given that 1 in 6 physicians at UW Medicine is a resident or fellow. |
For each of the six Strategic Values, our team has identified several Strategic Initiatives, to define the work we will do over the next six years to promote our values and improve the learning environment. It’s an ambitious plan.
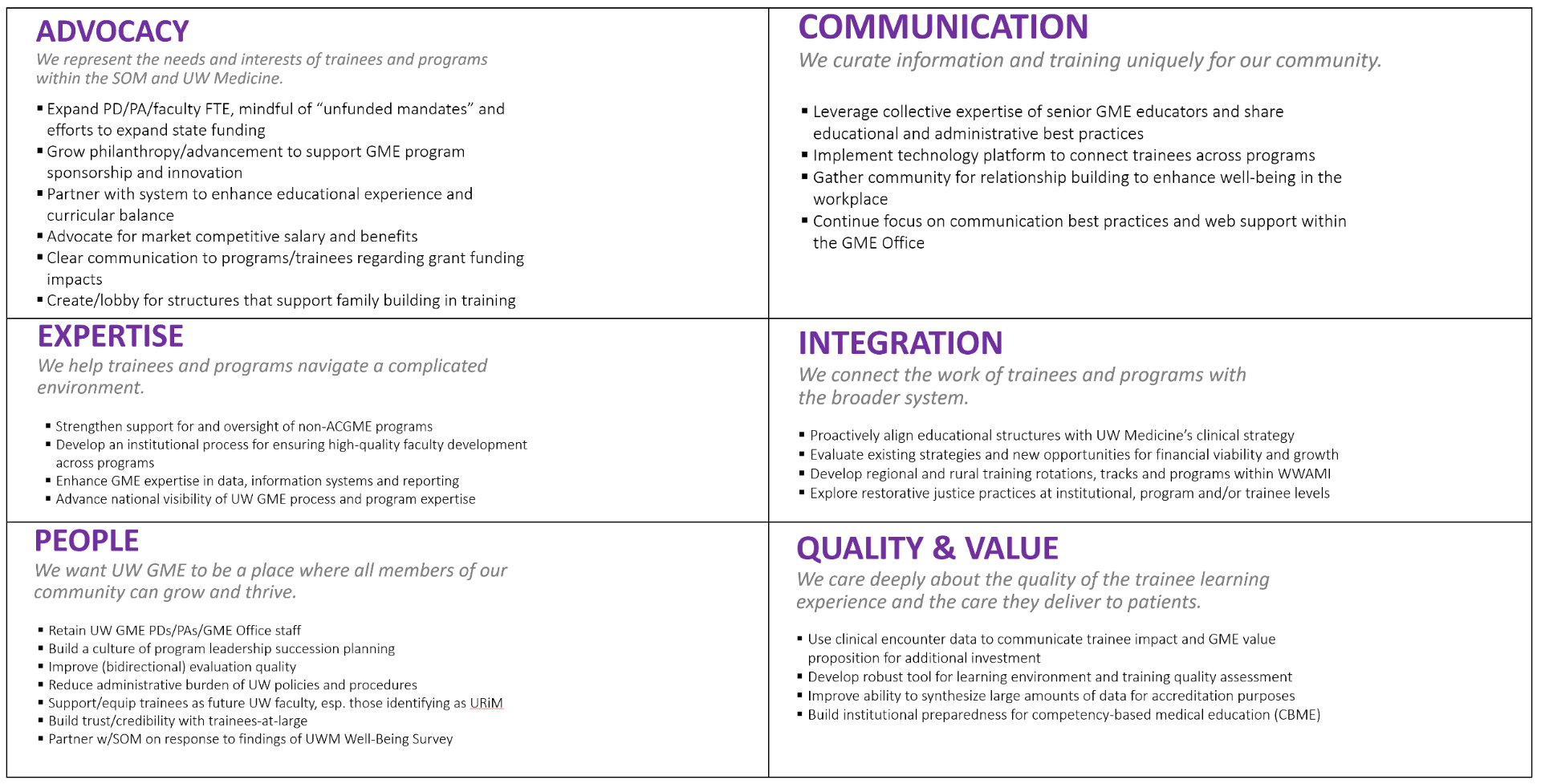
GME Leadership and team members are currently working on an implementation plan – to prioritize integration of this work into the enormous portfolio of work that we do every day to support residents, fellows, programs and departments. We invite colleagues from our community to join us in this work. In the next few months, we will share opportunities to participate in specific initiatives, but we also welcome your interest. Please reach out to Cindy Hamra (hamrac@uw.edu) if you’re interested in a specific area!
Finally, if you’re interested in learning more about this new GME Strategic Plan, this video featuring Cindy Hamra and Jennifer Best goes into more depth on each of the values, initiatives, and examples of the work to come.
 Byron Joyner, MD, MPA |
 Jennifer Best, MD |
 Cindy Hamra JD, MA |
Byron Joyner, MD, MPA
Vice Dean for GME and DIO
Jennifer Best, MD
Associate Dean, Accreditation and Education
Cindy Hamra, JD, MA
Associate Dean, Operations and Administration
by amande | Jul 20, 2023 | Announcements, Events, GME News & Notes, News

Dear GME Community,

Cindy Hamra Associate Dean, GME
A continued welcome this month from the GME Office to the 500+ new residents and fellows who are joining UW School of Medicine to start their clinical training. Dr. Joyner’s June blog post and The Huddle both celebrate new residents and fellows: Welcome 502 New Trainees.
July is Disability Pride Month, which honors “the history, achievements, experiences and struggles of the disability community in recognition of the anniversary of the Americans with Disabilities Act, landmark legislation that broke down barriers to inclusion in society” (see this WholeU article). The GME Office supports with trainees and programs regarding disability accommodations. Please reach out to Bre Smith, GME HR Manager, with any questions.
Finally, the Association for Hospital Medical Education has announced that August 18 is GME Professionals Day. Please take the time to thank colleagues in your departments and programs who support our 200+ graduate medical education programs here at the University of Washington School of Medicine.
The July issue of News & Notes includes lots of important information as we start the new academic year. If you have information you’d like included, please let me know.
Thanks,
Cindy
Policies and Processes
- Effective July 1, 2023, the GME Meals Policy and SCH Meals Policy have been updated to reflect an increase in meal reimbursement prices.
- In response to the recent Supreme Court decision on affirmative action for student admissions, President Cauce has provided a statement re-iterating the University of Washington’s commitment to creating opportunity and expanding access to world-class education for students from all backgrounds (Statement from UW President Ana Mari Cauce on the Supreme Court’s affirmative action decisions | UW News (washington.edu). We are currently working with the Attorney General’s Office to further analyze the Supreme Court’s decision and will follow up with more detailed information once that review is completed. Also sharing Follow-Up to Dr. Nasca’s June 13 Letter to the Community after Supreme Court Decision Regarding College Admissions and Race.
- The GMEPAC application for academic year 2024-2025 (AY25) is open and information is posted to the new GMEPAC webpage. Any changes in rotations or expansions that result in an increase in training time at any site requires pre-approval through the GMEPAC process and confirmation of funding by the hospital(s). The GMEPAC process does not include VA FTE. The GMEPAC process was discussed at the April 2023 Lunch & Learn and the presentation slides and recording are available. GMEPAC applications for AY25 are due July 28, 2023. Please reach out to Cindy Hamra or Amanda Easton if you have questions about the process or would like to discuss VA funding.
- GME Grant Funding Policy: The GME Office received feedback from our residents and fellows that late and/or conflicting information about grant funding availability and impacts has caused confusion and frustration. In response, we have developed a new Grant Funding Policy to centralize information and guidance that currently exists across multiple sources. We welcome your questions.
- The GME Office and GME Wellness are pleased to announce that as of July 1, 2023, the GME Wellness Service will be available to our non-ACGME fellows for those without faculty titles or with an existing counseling relationship. For those non-ACGME fellows with faculty titles (appointed as Acting Instructors), there are a number of support resources available via UWSOM Faculty Affairs. Please direct any questions to GME Director of Wellness, Dipti Chrastka.
- Learn More About Medical Regulation: The Federation of State Medical Boards has developed a series of educational modules to help medical students and residents learn about medical regulation before they begin their careers in medicine. The series includes:
- Residents and fellows who wish to moonlight must renew existing outside work activity requests for AY24. All requests for outside work must be reapproved each academic year. Please review the GME Outside Work webpage for the Moonlighting and Outside Work Policy and Outside Work Request Forms. Please email Angela James with any questions.
- Programs that have matched or extended an offer to a trainee who requires a disability accommodation should reach out to the GME Office (Bre Smith) as soon as possible so that we can work with the Disability Services Office to support the program and trainee through the process.
- The UW Medicine Bias Reporting Tool is for sharing incidents of bias including racism, sexism, ableism, discrimination of any form or other behaviors that do not reflect the prioritization of inclusion and equity expected in all areas of our community. Please feel free to share this flyer and postcard within your programs and workspaces.
- Additionally, the GME Concern Reporting tool is available to any members of the GME community to report concerns about the learning environment.
- Welcome New Program Administrators:
- Serena Wong, Headache Medicine, Movement Disorders, Neuro-Oncology, and Pediatric Neurocritical Care
- The GMEC has approved appointment of the following new program directors; ACGME appointments require Review Committee (RC) confirmation:
- Elizabeth Gass, Idaho Psychiatry
- Deepika Nehra, Surgical Critical Care
- The ACGME has a weekly e-Communication. If you wish to receive it, email ACGMECommunications@acgme.org.
Events of Interest
- GME Lunch & Learns
- AY24 Lunch and Learn schedule now posted
- July 20: ADS Annual Update + Program Oversight
- August 17: TBD
- UW Medicine Center for Scholarship in Patient Care Quality and Safety has shared the following information about application deadlines for key quality and safety training programs (apply via the Center website):
- August 3, 2023: Certificate Program in Quality and Safety: Designed for healthcare professionals and teams from all backgrounds. An outstanding development opportunity for your faculty and staff to mentor and execute QI projects.
- Other GME Events can be found on our calendar.
Projects and Resources
 The GME Office has posted an updated letter from Dr. Joyner for prospective residents and fellows to our GME Prospective Residents & Fellows page.
The GME Office has posted an updated letter from Dr. Joyner for prospective residents and fellows to our GME Prospective Residents & Fellows page.- As of this month, UW employees will have access to a new benefit with the Washington State Employee Assistance Program (WA EAP)—a free health and well-being program that is just for Washington state employees. The WA EAP replaces CareLink.
- UW Medicine Equity Impact Review Tool The UW Medicine Office of Healthcare Equity has developed an Equity Impact Review Tool to help with decisions about hiring, budgets, policies, procedures, and everyday issues. The tool leads decision-makers through a series of six steps that explicitly identify potential equity issues and initiates a process to produce more equitable outcomes. For more information, please visit the OHCE website.
- The GME Annual Program Timeline: Please review for important dates for July and August.
- Based on feedback from our community, in AY23 the GME Office developed Total Compensation sample statements for trainees at the R1 and R4 levels, meant to reflect incoming residents and incoming fellows, respectively. The R1 & R4 Total Compensation sample statements have been updated for AY24. These resources are posted to the GME Prospective Residents and Fellows page under a Compensation section, which also includes a Comparable Total Compensation Table summarizing how UW total compensation compares with other West Coast Institutions.
- Residents & Fellows – We want to hear from you! We hope to learn more about your current engagement with the UW GME Community and to understand opportunities for further connection and communication among trainees. Please take a moment to complete this survey and share your ideas about current and future GME education and community engagement events and tools.
- Residents and fellows are eligible to apply for a Housestaff Emergency Loan through the GME Office. The purpose of the loan fund is to provide emergency financial assistance to residents and fellows. The total amount of this loan has been increased from $1000 to $2500. Please see the loan form for complete details. As a reminder, our GME Financial Management for Residents & Fellows webpage is a great resource for trainees who would like to learn more about their finances and options as they prepare for graduation and a high-paying career.
- Trainees are encouraged to subscribe to UW Medicine STAT|INFO ADVISORY which has been designed to disseminate official information via text message to keep the UW Medicine workforce informed during emergencies and situations that might disrupt normal operations.
- A new opt-in module, Prioritizing Ourselves When Fatigued is a 5 minute training intended as a brief reminder on the important issue of fatigue. Learning Gateway is happy to answer any questions about the module.
- Our new Leave of Absence webpage is now live on the GME website. Here you will find LOA planning information and resources along with an intake form to contact GME for leave planning assistance: Leave Planning Submission Form. This form can be completed by trainees or program leadership. The December 2022 Lunch & Learn on ‘Leave Policy and Guidelines’ provides an overview of both these new resources; please the recording and slides.
People
- Jonathan Avery, resident, Internal Medicine, is lead author of “Risks factor and outcomes for isolated catheter-related deep venous thrombosis in patients undergoing allogeneic hematopoietic stem cell transplantation” in Thrombosis Research. Department of Medicine co-authors are Stephanie Lee and David Garcia.
- Joshua Bloomstein, resident, Internal Medicine, is co-author of “Impact of Gut Bacterial Metabolites on Psoriasis and Psoriatic Arthritis: Current Status and Future Perspectives” in the Journal of Investigative Dermatology.
- Physicians in the Cancer and Organ Transplant Clinic (COTC) at Fred Hutch recently published a report of a patient who became the 17th in the world to receive this life-saving therapy. “Until recently, the use of CAR T-cell therapy for PTLD had been largely unknown,” says Christopher Blosser, Transplant Nephrology Associate Program Director and COTC director. “Aggregated data from our case and the 16 previously published reports show this treatment is safe and effective. CAR T-cell therapy does not appear to cause organ rejection and has limited side effects when compared to other chemotherapies and immunotherapies.” Read the full story from Hutch News.
- Markus Boos, Dermatology Program Director, is featured in “More than skin in the game” from UW Medicine Newsroom.
- Kelley Branch, Cardiovascular Disease Associate Program Director, and Bryce Johnson, fellow, Cardiology, were awarded a CoMotion Innovation Award for $50,000 for development of the Seattle Clinical Pathway Platform (SCiPP) to update and market the current Chest Pain Pathway as well as expand the Platform to other disease states.
- Kelley Branch, Cardiovascular Disease Associate Program Director, is senior author of “Associations between clinical characteristics of cardiac arrest and early CT head findings of hypoxic ischaemic brain injury following out-of-hospital cardiac arrest” in Resuscitation. Department of Medicine co-author is Nicholas Johnson.
- Anne Browning, Associate Dean for Well-Being, is featured in “How LGBTQ+ UW Medicine Employees Define Pride” from The Huddle.
- Justin Bullock, fellow, Nephrology, is co-author of “Editors as Gatekeepers: One Medical Education Journal’s Efforts to Resist Racism in Scholarly Publishing” in Academic Medicine.
- Justin Bullock, fellow, Nephrology, wrote “I Am a Physician Face of Affirmative Action — The Supreme Court’s ruling hurts, but still I have hope” in Medpage Today.
- Congratulations to Maria Cassera, VA Chief Medical Resident, who has been accepted into the 2023 American Association for the Study of Liver Diseases Foundation Emerging Liver Scholars Program, which residents the opportunity to explore hepatology as a career through educational and professional development programming, learning directly from leaders in the field, and networking with hepatology key opinion leaders and peers from around the globe.
- Adam Cheng, resident, Internal Medicine, and colleagues are interested in understanding how different types of DNA damage lead to oncogenesis. Their lab discovered that many of the mutations that lead to cancerous cell behavior result from cellular misregulation of mutagenic enzymes, specifically a 7-member family of APOBEC enzymes. Learn more on the residency website.
- Congratulations to Roxanne Hicks, resident, Internal Medicine, and Rebecca Stephens, acting instructor, General Internal Medicine, this year’s recipients of the Tina Juul-Dam Primary Care Award, voted on by the medicine residents. The award memorializes Dr. Juul-Dam, a third-year resident who died in 2004 while on rotation in Alaska, and celebrates her spirit, dedication to patients, passion for primary care, and motivation of others.
- Christine Johnston, Infectious Diseases Associate Program Director, and Joshua Schiffer, professor, Allergy and Infectious Diseases, are co-authors of “Recurrent infection transiently expands human tissue T cells while maintaining long-term homeostasis” in the Journal of Experimental Medicine. Schiffer also wrote the editorial “The Continuing Puzzle of Defining Duration of Severe Acute Respiratory Syndrome Coronavirus 2 Infectivity” in the Journal of Infectious Diseases.
- Whitney Kiker, fellow, Pulmonary, Critical Care and Sleep Medicine, has been selected for the American Academy of Hospice and Palliative Medicine Research Scholars Program. This program aims to advance the scientific endeavors of new/early investigators (who have applied for or will shortly apply for a Career Development Award) whose goal is to become independent scientists actively involved in palliative care research.
- Nicole Kim, fellow, Gastroenterology, is lead author, and George Ioannou, professor, Gastroenterology, is senior author of “Addressing racial and ethnic disparities in US liver cancer care” in Hepatology Communications. Department of Medicine co-authors are Anne Cravero, Philip Vutien, Rotonya Carr, and Rachel Issaka.
- Linzee Mabrey, fellow, Pulmonary Critical Care, is lead author, and Mark Wurfel, professor, Pulmonary, Critical Care and Sleep Medicine, is senior author of “Phase 2, randomized, double-blind, placebo-controlled multi-center trial of the clinical and biological effects of anti-CD14 treatment in hospitalized patients with COVID-19 pneumonia” in EBioMedicine. Department of Medicine co-authors are Carmen Mikacenic, Eric Morrell and Thomas Martin.
- Chris Marfo, fellow, Surgical Critical Care is the winner of this year’s Harborview Medical Center Annual Housestaff Achievement Award for Clinical Ability and Humanitarian Concern.
- Tanya Meyer, Otolaryngology Program Director, and Neel Bhatt, co-authored recently published research that confirmed their suspicion: Some people with laryngeal dystonia and essential tremor of the vocal tract benefit from Botox injections more frequently than the three-month interval that most health insurers allow. Read the full story in the UW Medicine Newsroom.
- Natalia Murinova, Headache Program Director, is featured in “Migraine Aura or Stroke? When to Worry and What to Do” from Right as Rain by UW Medicine.
- Chloe Peters, resident, Urology, is featured in “ Peters highlights additional research on the effect of the Dobbs ruling on urologists” from Urology Times.
- Sarah Prager, Complex Family Planning Program Director, is featured in “Idaho patients traveling to Kennewick, WA, for abortions since ban” from The Bellingham Herald and in “Number of Idaho abortion patients traveling to Washington up 56% after Roe overturned” from Oregon Public Broadcasting. She is also featured in “Pence would ban abortions when pregnancies aren’t viable — his GOP rivals won’t say if they agree” from the Associated Press and “FDA approves the first over-the-counter birth control pill, Opill” from NPR.
- Bonnie Ronish, Occupational and Environmental Medicine Associate Program Director, is quoted in “Wildfires a threat to Seattle air quality again this year” from MyNorthwest.
- In the latest Thrivecast, “What it Means to be Patient and Family Centered,” Anneliese Schleyer, Interim Chief Medical Officer for UW Medicine, brings insight on what it means to center patients and families in the work we do. Hosted by Trish Kritek, Thrivecast provides tips to help clinicians, educators, and researchers thrive professionally in their careers, covering topics from time management and organization to leadership and self-advocacy.
- Ginny Ryan, Reproductive Endocrinology and Infertility Program Director, is featured in Opinion: Who gets to use the title ‘doctor’? from
- Congratulations to Amanda Shepherd, Internal Medicine Associate Program Director, who is the recipient of the 39th annual Paul B. Beeson Award. She was chosen by the medicine residents in recognition of outstanding clinical teaching and for exemplifying scholarship, humility, compassion, and integrity. The award commemorates Paul Beeson, a distinguished physician at the Seattle VA in the 1970s, who was celebrated for his teaching skills.
- Ken Steinberg has accepted the newly created position of Department of Medicine Vice Chair for Education, effective August 1. He has been program director for the Internal Medicine residency program since 2007.
- Rafee Talukder, fellow, Medical Oncology, received a 2023 John Quale Travel Fellowship from the Bladder Cancer Advocacy Network. The Travel Fellowship Program engages early-career individuals, such as basic scientists, urologists, oncologists, and pathologists, and connects them with hundreds of other bladder cancer research and medical professionals at the Bladder Cancer Think Tank annual meeting.
- Mark Wiley, postdoctoral scholar, and Jessica Bauer, research scientist, are co-lead authors and Barbara Jung, Department of Medicine Chair, is senior author of “Non-Canonical Activin A Signaling Stimulates Context-Dependent and Cellular-Specific Outcomes in CRC to Promote Tumor Cell Migration and Immune Tolerance” in Cancers.
by amande | Jul 7, 2023 | Announcements, News
Welcome!
 Byron Joyner, MD, MPA |
 Jennifer Best, MD |
 Cindy Hamra JD, MA |
We are excited that you are here to begin the next phase of your medical or dental education with us. Many of you have traveled from around the country – and from around the world – to train at the University of Washington School of Medicine.
We have all faced challenges and uncertainty, especially the last 3 years due to the COVID-19 pandemic and racial unrest. Many of you have never been to Seattle and might have questions as to whether this will be the right home for you. As you start your new journey, we want you to know that we are here for you. A world-class faculty and staff are committed to teaching you, providing you skills and feedback along the way. We want you to gain all the experiences you can and have all the learning opportunities you need to do your work. We want you to feel that you are working in a diverse learning environment, one that is inclusive, equitable, and fair.
There will be uncertainty during your training, not only because you will be learning new things about your chosen specialty but because uncertainty challenges you to discover new things about your community and the world. You will meet your colleagues and find new friends. You will encounter new interdisciplinary teams with whom you will care for patients, and, along the way, you will learn more about yourself.
Matriculating now into your new residency or fellowship program should be an adventure – even for those of you who are UW alumni returning as subspecialty fellows. Our top priority is to offer you the best and safest clinical learning environment so that you can develop the skills, behaviors, and attitudes you will need to be a successful, independent doctor.
You are one of the amazing, high-caliber physicians/dentists training in one of our 200+ residency and fellowship programs. This sets UW apart from other institutions. The new wave of 502 residents and fellows is our largest entering class ever. You represent an exceptional, diverse, and exceedingly qualified member of that class who will enrich each other’s lives and learning experiences. Best of luck to you!
Who you are
Exceptional.
- In total, you are 502 incoming residents and fellows
- You are pursuing 118 ACGME accredited specialties, over 85 non-ACGME specialties and 4 dental specialties
- 295 of you are first year residents
Many US medical school graduates going into your specialty have applied to our UW training programs, and you are among the select few to be admitted to our very competitive programs.
Diverse.
Altogether, you are global citizens who have studied around the world, with an increase in countries represented since last academic year:
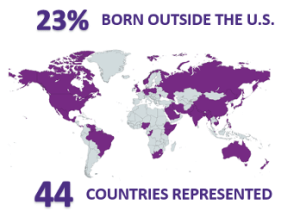

You show diversity in gender identity, representing an increase in female and non-binary trainees:
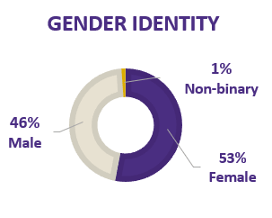
This is no accident. Diversity and inclusion are core values of UW Graduate Medical Education.
Qualified.

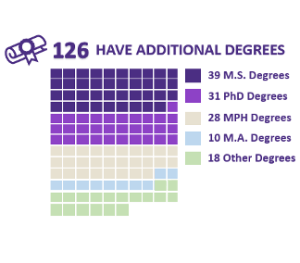
Where you are:
Graduate Medical Education (GME). GME programs sponsored by the UW School of Medicine are designed to train skillful physicians with ingrained habits of life-long learning and well-formed ethical and professional modes of practice.
UW Medicine. Among nearly 871 institutions, UW Medicine ranks seventh in the number of programs accredited by the Accreditation Council for Graduate Medical Education (ACGME), and ninth in the number of trainees.
Looking at the number for the 2023-2024 academic year:
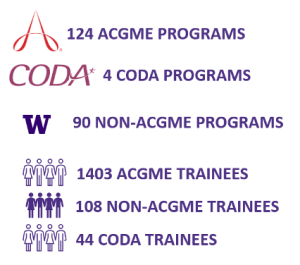
Although trainees most commonly rotate at Harborview Medical Center, the University of Washington Medical Center-Montlake & Northwest, Seattle Children’s Hospital, and the Veteran’s Administration, we partner with over 500 training sites throughout the WWAMI region – and the world – so you can have the best training.
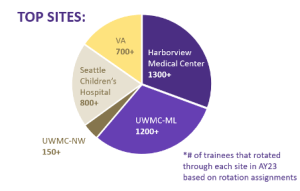
Who we are
GME Office. In partnership with many members of the learning community, we are responsible for the administrative oversight and academic quality of UW’s residency and clinical fellowship programs. Most importantly, we are here for you. Please contact any of us with questions, comments, or concerns. (http://gme.washington.edu/).
Congratulations and thank you!
Byron Joyner, MD, MPA
Vice Dean for GME and DIO
Jennifer Best, MD
Associate Dean, Accreditation and Education
Cindy Hamra, JD, MA
Associate Dean, Operations and Administration
by amande | Jun 21, 2023 | Announcements, News, Sticky
 As the new academic year begins, 502 new residents and fellows are joining UW Graduate Medical Education (GME) programs to further their medical and dental training.
As the new academic year begins, 502 new residents and fellows are joining UW Graduate Medical Education (GME) programs to further their medical and dental training.
Graduate medical education refers to the period of education in a particular specialty (residency) or subspecialty (fellowship) following medical or dental school. Here, trainees work in hundreds of different programs, from emergency medicine and surgery to lesser-known specialties such as nuclear medicine and headache medicine.
One in six physicians at UW Medicine is a resident or fellow, and over 100 graduating residents and fellows accept faculty roles within UW Medicine each year.
“It is always a pleasure to welcome new residents and fellows to our UW Medicine family. Every year, we look forward to training the next generation of exceptional physicians and to their many contributions to our patients — and to improving the health of all people,” says Byron Joyner, MD, vice dean for Graduate Medical Education and a Designated Institutional Official.
Read more >
by amande | Jun 23, 2023 | Announcements, Events, GME News & Notes, News

Dear GME Community,

Cindy Hamra Associate Dean, GME
First, a sincere welcome from the GME Office to the 500+ new residents and fellows who are joining UW School of Medicine to start their clinical training. GME hosted New Resident and Fellow Orientation on Wednesday to kick off the new academic year. The Huddle also featured an article about our new residents and fellows: Welcome 502 New Trainees.
We also want to wish our graduating residents and fellows the best as they move to the next stages of their careers.
June is Pride Month, when we celebrate the history, diversity and contributions of LGBTQIA people in the United States. For more about the history of Pride Month and what how UW Medicine does to honor and recognize the month (including digital assets and posters) please see the recent feature in The Huddle, as well as a spotlight on transgender voices from The Whole U.
The June 2023 edition of News & Notes has a lot of information about ongoing projects, new and updated policies, and pending events.
Thanks,
Cindy

Policies and Processes
- *New* GME Grant Funding Policy: The GME Office received feedback from our residents and fellows that late and/or conflicting information about grant funding availability and impacts has caused confusion and frustration. In response, we have developed a new Grant Funding Policy to centralize information and guidance that currently exists across multiple sources. We welcome your questions.
- The GME Office and GME Wellness are pleased to announce that as of July 1, 2023, the GME Wellness Service will be available to our non-ACGME fellows for those without faculty titles or with an existing counseling relationship. For those non-ACGME fellows with faculty titles (appointed as Acting Instructors), there are a number of support resources available via UWSOM Faculty Affairs. Please direct any questions to GME Director of Wellness, Dipti Chrastka.
- Learn More About Medical Regulation: The Federation of State Medical Boards has developed a series of educational modules to help medical students and residents learn about medical regulation before they begin their careers in medicine. The series includes:
- The GMEPAC application for academic year 2024-2025 (AY25) is open and information is posted to the new GMEPAC webpage. Any changes in rotations or expansions that result in an increase in training time at any site requires pre-approval through the GMEPAC process and confirmation of funding by the hospital(s). The GMEPAC process does not include VA FTE. The GMEPAC process was discussed at the April 2023 Lunch & Learn and the presentation slides and recording are available. GMEPAC applications for AY25 are due July 28, 2023. Please reach out to Cindy Hamra or Amanda Easton if you have questions about the process or would like to discuss VA funding.
- It is time for trainees to begin renewing their outside work activity requests for AY24. As a reminder, all requests for outside work must be reapproved each academic year. Please review the GME Outside Work webpage for the Moonlighting and Outside Work Policy and Outside Work Request Forms. Please email Angela James with any questions.
- Programs that have matched or extended an offer to a trainee who requires a disability accommodation, should reach out to the GME Office (Bre Smith) as soon as possible so that we can work with the Disability Services Office to support the program and trainee through the process.
- The AY24 GME Orientation webpage is now live! This webpage includes detailed information about important UW GME onboarding and orientation information. Additional pages with helpful information for trainees as they complete the onboarding process:
- The COVID-19 public health emergency is ending May 11, 2023. At the beginning of the COVID-19 public health emergency, CMS used emergency waiver authorities and various regulatory authorities to enable flexibilities so providers could rapidly respond to people impacted by COVID-19. Some of those flexibilities have been extended temporarily, some permanently, and some are ending on May 11. Please review resources on the UW Compliance COVID-19 Public Health Emergency page to answer questions you may have about changes impacting clinicians due to the end of the public health emergency.
- Please note the changes to University COVID-19 policies effective June 12th unless otherwise noted.
- The UW Medicine Bias Reporting Tool is for sharing incidents of bias including racism, sexism, ableism, discrimination of any form or other behaviors that do not reflect the prioritization of inclusion and equity expected in all areas of our community. Please feel free to share this flyer and postcard within your programs and workspaces.
- Additionally, the GME Concern Reporting tool is available to any members of the GME community to report concerns about the learning environment.
- Interpreter Services and the Office of Healthcare Equity have created an online guide dedicated to providing resources for accessing medical interpreters, tips for partnering with medical interpreters, reminders about laws and regulations and directions on what to do in emergencies. Please read more about Clear Communication: Every Patient, Every Time.
- The GMEC has approved appointment of the following new program directors; ACGME appointments require Review Committee (RC) confirmation:
- Ania Lang, Allergy & Immunology (ACGME)
- Evelyn Hsu, Pediatric Gastroenterology, Hepatology and Nutrition, (ACGME – Interim)
- The GMEC approved revisions to the following policies at the May meeting. All are posted on the Policies and Procedures page of the GME website.
- Grant Funding Policy (see above)
- Scheduling and Boarders Policy
- The ACGME has a weekly e-Communication. If you wish to receive it, email ACGMECommunications@acgme.org.
Events of Interest
- GME Lunch & Learns
- AY24 Lunch and Learn schedule now posted
- July 20: ADS Annual Update + Program Oversight
- GME Outreach Event for trainees at HMC on June 30th from 11am to 1 pm. We encourage trainees to stop by to say hello, meet our GME team members and take a packed lunch. Please look for an email closer to the event with specific room details.
- The Institute for Common Power in partnership and the University of Washington Department of Medicine will be holding their quarterly Diversity Lecture series on Tuesday, June 29th from 12:00pm PST to 1:00pm PST (3:00pm EST to 4:00pm EST). Please join for “The History and Future of Black Physicians in Medicine” with Dr. Walter Conwell, Morehouse School of Medicine. Learn more and RSVP.
- UW Medicine Center for Scholarship in Patient Care Quality and Safety has shared the following information about application deadlines for three key quality and safety training programs (apply via the Center website):
- June 30, 2023: QI Scholars Program: Competitive yearlong advanced training; designed for junior and mid-career faculty pursuing QI as a scholarly focus.
- June 30, 2023: GME Quality & Safety Foundations Course: Open to any UW Medicine GME program—helps meet ACGME requirements for Quality Improvement and Patient Safety.
- August 3, 2023: Certificate Program in Quality and Safety: Designed for healthcare professionals and teams from all backgrounds. An outstanding development opportunity for your faculty and staff to mentor and execute QI projects.
- Other GME Events can be found on our calendar.
Projects and Resources
 The GME Annual Program Timeline: Please review for important dates for June and July.
The GME Annual Program Timeline: Please review for important dates for June and July.- Based on feedback from our community, in AY23 the GME Office developed Total Compensation sample statements for trainees at the R1 and R4 levels, meant to reflect incoming residents and incoming fellows, respectively. The R1 & R4 Total Compensation sample statements have been updated for AY24. These resources are posted to the GME Prospective Residents and Fellows page under a Compensation section, which also includes a Comparable Total Compensation Table summarizing how UW total compensation compares with other West Coast Institutions.
- Residents & Fellows – We want to hear from you! We hope to learn more about your current engagement with the UW GME Community and to understand opportunities for further connection and communication among trainees. Please take a moment to complete this survey and share your ideas about current and future GME education and community engagement events and tools.
- Residents and fellows are eligible to apply for a Housestaff Emergency Loan through the GME Office. The purpose of the loan fund is to provide emergency financial assistance to residents and fellows. The total amount of this loan has been increased from $1000 to $2500. Please see the loan form for complete details. As a reminder, our GME Financial Management for Residents & Fellows webpage is a great resource for trainees who would like to learn more about their finances and options as they prepare for graduation and a high-paying career.
- Trainees are encouraged to subscribe to UW Medicine STAT|INFO ADVISORY which has been designed to disseminate official information via text message to keep the UW Medicine workforce informed during emergencies and situations that might disrupt normal operations.
- A new opt-in module, Prioritizing Ourselves When Fatigued is a 5 minute training intended as a brief reminder on the important issue of fatigue. Learning Gateway is happy to answer any questions about the module.
- Our new Leave of Absence webpage is now live on the GME website. Here you will find LOA planning information and resources along with an intake form to contact GME for leave planning assistance: Leave Planning Submission Form. This form can be completed by trainees or program leadership. The December 2022 Lunch & Learn on ‘Leave Policy and Guidelines’ provides an overview of both these new resources; please the recording and slides.
People
- GME Team Members received Wellbeing Grant Funding for the following projects:
- Therapeutic Lightboxes for Resident Well-Being Project (submitted by the GME Wellness Team): This project aims to improve resident wellness by equipping windowless work and team rooms at identified hospital sites with therapeutic lightboxes (10,000 lux). With Seattle’s long dark winters and limited hours of sunlight, light therapy can improve mood, combat fatigue, regulate sleep cycles, increase focus, and contribute to stress reduction and enhanced resident well-being. Thanks to Tara Reid, faculty, Infectious Diseases, for the suggestion!
- GME Staff Community Series (submitted by the GME Office Professional Development Group): This project aims to create opportunities for staff across GME’s diverse departments to come together, connect, and celebrate each other and the work we do. These events include outdoor celebrations, indoor arts, and more. Our goal is to continue building and maintaining the relationships that enrich our lives and help us to continue to improve our world-class support to our physician-learners.
- The EDItorial is a monthly Equity, Diversity, and Inclusion Awareness Newsletter created by Internal Medicine residency program staff. Each month they highlight different marginalized groups with opportunities to engage, support, and participate on international, national, and local levels. The June newsletter highlights pride month and the LGBTQIA+ community. Read the EDItorial on the IM residency website.
- Emily Brown, Associate Program Director, Child Abuse Fellowship is featured in ‘Public Health Emergency ends – so does Medicaid automatic re-enrollment‘ from Northwest Asian Weekly.
- Daniel Cabrera, Associate Program Director, Internal Medicine Residency, is co-author of “Everyone Deserves to Belong” in The Hospitalist.
- Jason Castaneda, R2, Internal Medicine, is quoted in “Insomnia Drug Class May Not Influence Exacerbation Risks in COPD Patients” in Sleep Review.
- Jason Castaneda, R2, Internal Medicine and Lucas Donovan, assistant professor (Pulmonary, Critical Care and Sleep Medicine) are quoted in “Mortality, exacerbation risk in patients with COPD not higher with insomnia hypnotics” in Healio Pulmonology.
- Tom Fitzpatrick, fellow, Allergy and Infectious Diseases, is quoted in “Council rejects Davison’s push to prosecute drug possession and public use” from Real Change.
- The Curbsiders Internal Medicine podcast featured top pearls from the recent Society of General Internal Medicine annual meeting, including Barak Gaster, professor, General Internal Medicine, for “Dementia in Primary Care” and Rebecca Gold R2, Internal Medicine and Adelaide McClintock, assistant professor, General Internal Medicine for “Trauma-Informed Care.”
- Mary Geist, R1, Internal Medicine, is lead author and Jocelyn James, assistant professor (General Internal Medicine) is senior author of “Timing of hepatitis C treatment initiation and retention in office-based opioid treatment with buprenorphine: a retrospective cohort study” in Addiction Science and Clinical Practice. Department of Medicine co-authors are Andrea Radick, Judith Tsui, and Nancy Connolly.
- Melissa Herrin, Chief Resident, Occupational and Environmental Medicine, recently published ‘Work, Service and Health: Lessons from Veterans in the Environmental Contaminants Clinic’ in the health policy section of in-House: The Agora for Medical Residents and Fellows. She describes her training experience at the VA Puget Sound and advocates for health benefits for veterans with exposure concerns.
- Christopher Hofstetter, Associate Program Director, Spine Surgery, is featured in “Ultra Minimally Invasive Spine Surgery” from The Huddle.
- Zaroug Jaleel, resident, Otolaryngology, is recipient of the 2023 AAO-HNSF Resident Research Award.
- Nicholas Johnson, Associate Program Director, Critical Care Medicine, is co-author of “Changing Severity and Epidemiology of Adults Hospitalized With Coronavirus Disease 2019 (COVID-19) in the United States After Introduction of COVID-19 Vaccines, March 2021-August 2022” in Clinical Infectious Diseases.
- Barbara Jung, Chair, Department of Medicine, is the current America Gastroenterological Association President. Read more about her role and how she is paving the way for women in gastroenterology.
- Vishesh Kapur, Program Director, Sleep Medicine, is quoted in “Wide Awake at Bedtime Despite Being *So* Sleepy Mid-Afternoon? Here’s What To Know About Catching a ‘Second Wind’ of Energy” from Well+Good.
- Hiba Khan, fellow, Medical Oncology, received a 2023 Young Investigator awards from the American Society of Clinical Oncology for “Dismantling Disparities in Access to Oral Novel Hormonal Therapies in Prostate Cancer–A Mixed-Methods Analysis from a Population, Systems, and Patient-Centered Lens.”
- Among people whose liver is failing, the perpetual shortage of donor organs inhibits expectations of a timely, life-saving transplant. New research suggests that these people who initially seek care at safety-net hospitals may face additional obstacles to being considered for transplant. A study of three safety-net hospitals showed that, among patients whose measures of liver health would typically result in a referral for transplant evaluation, only about one-fourth received the referral. The finding was published June 8 in JAMA Network Open. “Patients who receive care at these safety-net hospitals generally do not go to the other hospital unless they have a specific referral,” said Nicole Kim, a co-author on the paper and a liver transplant fellow at the University of Washington School of Medicine. “Patients who present at safety-net hospitals are often more likely to identify as indigent and underserved, uninsured, lower-income, racial-ethnic minority and-or homeless.” Read the full story from UW Medicine Newsroom.
- Somnath Mookherjee, Program Director, Academic Hospitalist Fellowship, is the recipient of the 2023 National Award for Scholarship in Medical Education from the Society of General Internal Medicine. He received the award for his extensive body of scholarly work related to clinical teaching and evidence-based physical exam that has impacted medical education across the spectrum from UME to GME to CME, and also his successful mentoring in educational scholarship and demonstration of educational leadership.
- Leo Morales, professor and Assistant Dean for UW School of Medicine, has been invited to serve as a member of the National Advisory Council (NAC) subcommittee for the Agency for Healthcare Research and Quality (AHRQ). The goal of this subcommittee is to make recommendations to the NAC on AHRQ’s proposed long-term strategic planning for AHRQ’s Patient-Centered Outcomes Trust Fund (PCORTF) investments.
- Fernando Picazo, fellow, Pulmonary, Critical Care and Sleep Medicine, is a 2023 recipient of the Underrepresented Trainee Development Scholarship from the American Thoracic Society (ATS).
- Jeff Probstfield, professor, and Kelley Branch, Program Director, Cardiovascular Disease, are co-authors of “Global Variations in Heart Failure Etiology, Management, and Outcomes” in
- Paul Pottinger, Program Director, Infectious Diseases, is quoted in “Rabid bat found in E. WA. It was the first in 5 years in Tri-Cities-Walla Walla region” in the Tri-City Herald.
- Ganesh Raghu, Program Director, Interstitial Lung Disease, is senior author of “Lung parenchymal abnormalities and outcomes in hospitalized patients with COVID 19 pneumonia: A positive message from a prospective hospital-based longitudinal study for future considerations” in Respiratory Medicine.
- Colbey Ricklefs, Resident, Family Medicine received the 2023 Mizzou Alumni Association – Young Alumni Award.
- Maureen Ryan-Murphy, Chief Resident, Psychiatry, is featured in ‘At the intersection of homelessness, mental illness and addiction in Portland lies psychosis’ from KGW8.
- Talicia Savage, R3, Internal Medicine, is lead author and Rachel Issaka, assistant professor (Gastroenterology) is senior author of “Association between patient, clinic, and geographical-level factors and 1-year surveillance colonoscopy adherence” in Clinical and Translational Gastroenterology. Department of Medicine co-authors are Veena Shankaran and Scott Ramsey.
- The Spring 2023 edition of Surgery Synopsis includes a wealth of information including features of newly appointed Vice Chairs, Program Directors, and trainees.
- Thomas Walsh, Program Director, Andrology, is featured in ‘Men’s Health Center Provides Comprehensive Care’ from The Huddle.
- Natalie Weathered, Program Director, Neurology, is featured in ‘If the Brain Is a Puzzle, Natalie Weathered Wants to Solve It’ from The Huddle.
- Douglas Wood, Chair, Department of Surgery, received the National Comprehensive Cancer Network’s (NCCN) 2023 Rodger Winn Award for decades of work to develop, refine and promote the organization’s Clinical Practice Guidelines in Oncology.
by amande | Jun 2, 2023 | Announcements, News
-
-
 Jennifer Best, MD |
 Cindy Hamra JD, MA |
 Byron Joyner, MD, MPA |
|
|
Dear Graduating Residents and Fellows,
Longer days and the reemerging sunshine are reminders that we are nearing the end of another academic year. For you, this year brings a remarkable accomplishment – completion of the residency and/or fellowship training that brought you to the University of Washington.
Simply put, thank you. Thank you for trusting UW Medicine with your development. Thank you for your commitment to learning, despite the crises of the pandemic and societal unrest. Thank you, most of all, for the big and small ways you cared for your patients – and for one another – in these trying times.
May the coming weeks bring meaningful celebrations with your colleagues, your faculty and staff, and those that you love.
On behalf of the GME team, it is a privilege to tell you how proud we are of each of you. We join your programs in honoring the many gifts you will offer the world. Your future is bright!
Congratulations!
- Jennifer Best, MD
Associate Dean, Accreditation and Education
- Cindy Hamra, JD
Associate Dean, Operations and Administration
-
- Byron Joyner, MD, MPA
Vice Dean for GME and DIO
by amande | May 19, 2023 | Announcements, Events, GME News & Notes, News
Dear GME Community,

Cindy Hamra Associate Dean, GME
Like many of you, the GME Office is busy this time of year, onboarding our nearly 500 incoming residents and fellows, planning for orientation, working on graduation certificates and planning for the new academic year. We also celebrate Asian, Native Hawaiian and Pacific Islander Heritage Month. The Huddle has put together great resources and information.
We are also excited to be launching our new Strategic Plan for AY24-29. We will be presenting this plan to various groups and committees and a recording of the 5/18 Lunch & Learn (starts at 48:30) is available to the community. Thanks to those of you who gave feedback and otherwise contributed!
Please make sure to check News & Notes for reminders of the many processes and deadlines that are relevant this time of year, and don’t hesitate to contact our office with questions or for support.
Thanks,
Cindy

Policies and Processes
- The GMEPAC application for academic year 2024-2025 (AY25) is open and information is posted to the new GMEPAC webpage. Any changes in rotations or expansions that result in an increase in training time at any site requires pre-approval through the GMEPAC process and confirmation of funding by the hospital(s). The GMEPAC process does not include VA FTE. The GMEPAC process was discussed at the April 2023 Lunch & Learn and the presentation slides and recording are available. GMEPAC applications for AY25 are due July 28, 2023. Please reach out to Cindy Hamra or Amanda Easton if you have questions about the process or would like to discuss VA funding.
- It is time for trainees to begin renewing their outside work activity requests for AY24. As a reminder, all requests for outside work must be reapproved each academic year. Please review the GME Outside Work webpage for the Moonlighting and Outside Work Policy and Outside Work Request Forms. Please email Angela James with any questions.
- Programs that have matched or extended an offer to a trainee who requires a disability accommodation, should reach out to the GME Office (Bre Smith) as soon as possible so that we can work with the Disability Services Office to support the program and trainee through the process.
- The AY24 GME Orientation webpage is now live! Incoming trainees have been advised to visit this webpage for detailed information about important UW GME onboarding and orientation information. This page will be updated between now and the start of AY24 appointments, so we encourage trainees and programs to check back frequently for updates. In addition to our main orientation page, we would also like to highlight other pages which will have helpful information for trainees as they complete the onboarding process and prepare for our live orientation event on June 21st from 8:00 am – 1:00 pm PST:
- The COVID-19 public health emergency is ending May 11, 2023. At the beginning of the COVID-19 public health emergency, CMS used emergency waiver authorities and various regulatory authorities to enable flexibilities so providers could rapidly respond to people impacted by COVID-19. Some of those flexibilities have been extended temporarily, some permanently, and some are ending on May 11. Please review resources on the UW Compliance COVID-19 Public Health Emergency page to answer questions you may have about changes impacting clinicians due to the end of the public health emergency.
- Please note the changes to University COVID-19 policies effective June 12th unless otherwise noted.
- The UW Medicine Bias Reporting Tool is for sharing incidents of bias including racism, sexism, ableism, discrimination of any form or other behaviors that do not reflect the prioritization of inclusion and equity expected in all areas of our community. Please feel free to share this flyer and postcard within your programs and workspaces.
- Additionally, the GME Concern Reporting tool is available to any members of the GME community to report concerns about the learning environment.
- Interpreter Services and the Office of Healthcare Equity have created an online guide dedicated to providing resources for accessing medical interpreters, tips for partnering with medical interpreters, reminders about laws and regulations and directions on what to do in emergencies. Please read more about Clear Communication: Every Patient, Every Time.
- The University of Washington continues to require facemasks in healthcare and clinical facilities after the statewide healthcare mask order from the Washington State Secretary of Health ends on April 3, 2023. This decision is in alignment with UW Medicine’s medical facilities, our public health partners and other local health systems.
- The GMEC has approved appointment of the following new program directors; ACGME appointments require Review Committee (RC) confirmation:
- Andrew Koth, Pediatric Critical Care Medicine fellowship (ACGME)
- Judith Hagedorn, Urology residency (ACGME)
- In response to recent concerns about known precedent of unprofessional behaviors, the GME Office has modified the Program Director Change/Appointment Request Letter Template to include the following language:
- Acknowledging that a program director must be a role model of professionalism (ACGME CPR II.A.4.a), I personally attest that I have not been made aware of prior or current concerns regarding Dr. <<Last Name>> ‘s professional or ethical behaviors toward trainees, faculty, staff, or patients.
- The ACGME has a weekly e-Communication. If you wish to receive it, email ACGMECommunications@acgme.org.
Events of Interest
- Please mark your calendars for the Annual GME AY24 Event Calendar. As always, the GME Website remains the best way to get the most up-to-date information. Check out the PD & PA, and Resident & Fellow pages for info on upcoming and past events including resources and recordings (if applicable). Email reminders, Zoom links and registration information (if required) will be sent via email as individual events approach. Please note that attendance at the bi-annual Program Director Development Series (PDDS) is a requirement for all ACGME programs.
- Upcoming GME Lunch & Learns
- Residents and fellows are invited to join the School of Medicine strategic planning listening session on Wednesday, May 24th from 5.30 – 6.30pm.
- Our final Chief Resident and Fellow Listening Session for the academic year will be held on Thursday, June 1st from 5:00 – 6:00 pm. Chiefs will have received an email with session details from the GME Office and we ask that program leadership support Chiefs in attending.
- Other GME Events can be found on our calendar.
People
- EDItorial: Asian Pacific American Heritage Month: The EDItorial is a monthly Equity, Diversity, and Inclusion Awareness Newsletter created by the Internal Medicine (IM) residency program staff. Each month they highlight different marginalized groups with opportunities to engage, support, and participate on international, national, and local levels. The May newsletter highlights Asian Pacific American Heritage Month. Read the EDItorial on the IM residency website.
- Emergency Medicine residents are featured in UW Law Students ‘Depose’ UW Emergency Medicine Residents.
- Atrial fibrillation, “AFib”, is the most common heart arrhythmia in adults and is projected to affect 12 million U.S. residents by 2030. About 70% of people with atrial fibrillation are 65 to 85, a population demographic projected to grow over the next few decades. Nazem Akoum, Clinical Cardiac Electrophysiology Program Director, specializes in ablation. Read the full story from UW Medicine Newsroom.
- Nazem Akoum, Clinical Cardiac Electrophysiology Program Director, is quoted in “New Risk Factors, Better Treatments for AFib: What to Know” from WebMD.
- Dermatology residents Mariam Alam and Caitlin Crimp are organizing patient panels as part of their collaborative research project, “Mitigating Bias and Burnout Through Patient-Centered Narrative Medicine.” In June 2022, they received a grant through the Accreditation Council for Graduate Medical Education’s (ACGME) Back to Bedside program to develop a narrative medicine curriculum for dermatology residents, with the goal to improve residents’ understanding and connection to patients and mitigate both bias and burnout. Narrative Medicine is an emerging approach to health care that draws on the study of art and literature to enhance listening and observation skills. Read the full story on the Dermatology website.
- Katherine Bennett, Geriatric Medicine Program Director, has been elected Chair of the Fellowship Director’s Group for the American Geriatrics Society/Association of Directors of Geriatric Academic Programs. She will serve a three-year term, chair the Fellowship Director’s Preconference and represent the fellowship program director’s at society board meetings.
- Kelley Branch, Cardiovascular Disease Associate Program Director, is lead author of “Diagnostic yield, safety, and outcomes of head-to-pelvis sudden death CT imaging in post arrest care: The CT FIRST cohort study” in Resuscitation. Department of Medicine co-authors are Peter Kudenchuk, Jeff Probstfield, David Carlbom, and Nicholas Johnson.
- Justin Bullock, fellow, Nephrology, is co-author of “My Assessments Are Biased!” Measurement and Sociocultural Approaches to Achieve Fairness in Assessment in Medical Education” in Academic Medicine.
- Anna Condella, fellow, Pulmonary, Critical Care and Sleep Medicine, is lead author of “Veno-venous Extracorporeal Membrane Oxygenation for COVID-19: A Call For System-Wide Checks to Ensure Equitable Delivery For All” in ASAIO Journal.
- Kirk Deene, Associate Program Director, Neuropathology, is quoted in “Tracking King County seniors (and their brains) for clues to dementia and Alzheimer’s” in The Seattle Times.
- Jonathan Harper, Endourology Program Director, is featured in Kidney stone breakthrough procedure at UW called ‘game changer’ for patients from KOMO.
- Lianne Hirano, Palliative Medicine Program Director, is quoted in “’A different animal’: Doctors warn seniors about potency of cannabis products” from KOMO News.
- Christine Johnston, Infectious Diseases Associate Program Director, is quoted in “Tired of ‘dead end’ approach, herpes patients mobilize to demand government action” in STAT.
- Aditya Joshi, fellow, Cardiology, is co-author of “The Relationship between Circulating Apolipoprotein A-1 and Atherosclerosis Initiation and Progression in Psoriasis” in the Journal of Investigative Dermatology.
- Hiba Khan, Noam Kopmar, Chipo Kwendakwema, and Emily Liang, Hematology-Oncology fellows, have received merit awards from the American Society of Cancer Organization (ASCO). Merit Awards support students and trainees who are first authors on abstracts selected for presentation at the ASCO Annual Meeting.
- Hiba Khan, fellow, Hematology-Oncology, is lead author and Veena Shankaran, professor (Medical Oncology) is senior author of “Financial Toxicity in Cancer Care: Implications for Clinical Care and Potential Practice Solutions” in Journal of Clinical Oncology. Department of Medicine co-author is Scott Ramsey.
- Amy Law, Instructional Designer on the GME Team, presented a workshop called “Using Empathy Maps to Investigate Complex Problems” at the AAMC Western Group Collaborative Spring Conference in April. The workshop focused on using a design thinking tool to investigate the variety of stakeholder perspectives and needs related to complex problems like mistreatment in medical education. Amy co-presented with Ceradwen Tokheim from SOMALT.
- Joseph Merrill, Addiction Medicine Program Director, is featured in Is moderate drinking good for your health? from KING 5 News. He is also quoted in “‘They saved my life’: Everett man credits Harborview addiction program with helping him get sober” from KIRO News.
- Chinenyenwa Mpamaugo, resident, Pediatrics, is featured in Tips to keep your kids safe on the water with warmer weather from KXLY.
- Chloe Peters, resident, Urology, is the resident recipient of the Dr. Reem Ghalib Award for Promotion of Gender Equity. The award, named in honor of Dr. Reem Ghalib, a renowned advocate for women in medicine, was established in 2020 by Dr. Ghalib’s colleagues to recognize her dedication to improving the pathway for women medical trainees. “Dr. Peters is an outstanding early-career urologist who has made significant contributions to the field, and we are excited to see her present her research at the 2023 Annual Meeting of the American Urological Association. Urology is traditionally a male-dominated medical specialty and we are proud to support her important work,” said the award committee.
- Paul Pottinger, Infectious Disease Program Director, is quoted in “Can COVID-19 Cause Itchy Eyes or Pink Eye?” from Everyday Health.
- Sarah Prager, Complex Family Planning Program Director, is quoted in “Abortion pill legal challenge threatens miscarriage care” from the Associated Press.
- Shinetra Pryor, Program Administrator for Geriatric Medicine and Palliative Medicine, was invited to present on best practices for recruitment at the Fellowship Director’s Preconference at the American Geriatrics Society Meeting.
- Coralynn Sack, Occupational and Environmental Medicine Associate Program Director, is co-author of “Association between any underlying health condition and COVID-19-associated hospitalization by age group, Washington State, 2020-2021: a retrospective cohort study” in BMC Infectious Diseases. She is also quoted in “Exploitation, Abuse, and Death: The Dark Side of Working in the Weed Industry” in The Nation.
- Matthew Thau, former fellow, is lead author and Eric Morrell, assistant professor (Pulmonary, Critical Care and Sleep Medicine) is senior author of “Association of Trauma Molecular Endotypes With Differential Response to Transfusion Resuscitation Strategies” in JAMA Surgery. Department of Medicine co-authors are Ted Liu, Neha Sathe, W. Conrad Liles, Ian Stanaway, Carmen Mikacenic, Mark Wurfel, and Pavan Bhatraju.
- Matthew Thau, former fellow, is lead author and Pavan Bhatraju, assistant professor (Pulmonary, Critical Care and Sleep Medicine) is senior author of “Following the MAP for Improved Kidney Function in Hepatorenal Syndrome” in Kidney 360.
- Mitchell Vollger, fellow, Medical Genetics, is lead author of “Increased mutation and gene conversion within human segmental duplications” and co-author of “A draft human pangenome reference” in Nature. Learn more in “UW Medicine plays key role in NIH pangenome studies” from UW Medicine Newsroom.
- Lisa Vande Vusse, Internal Medicine Associate Program Director, wrote “White Hair Ritual” in the Journal of General Internal Medicine.
by amande | May 4, 2023 | Announcements, News

Byron Joyner, MD, MPA
This month, I’ve invited Hadar Duman, GME Director of Accreditation, to share her thoughts about the importance of the annual ACGME Resident and Faculty Surveys.
Byron Joyner, MD, MPA
Vice Dean for Graduate Medical Education, Designated Institutional Official

Hadar Duman, MHI Director of Accreditation
The 2023 ACGME Survey results are out! As an accreditation enthusiast, I am filled with excitement. The Surveys are an annual assessment of the experiences and opinions of residents, fellows, and faculty in ACGME-accredited programs. They serve as a vital tool for the ACGME to monitor and improve the quality of graduate medical education, expand the scope of trainees’ input in the accreditation process, and make annual accreditation and policy decisions based on systematic data collection and analysis. These Surveys also give us an opportunity to make changes based on the feedback we receive. The ACGME has been administrating the survey since 2004, and it was revised twice, in 2011 and 2020, to reflect current requirements. The Surveys’ importance has only increased over the years. This is especially true since the move to the Next Accreditation System (NAS) in 2011, when the frequency of site visits was reduced to once per decade. Absent of site visits, ACGME increased their reliance on survey data to make accreditation decisions.
However, despite the high stakes of the survey, the ACGME keeps the survey questions confidential. Programs do their best to prepare trainees and faculty so they understand the meaning of the questions and content areas, but the truth is that programs go at it blind. This leaves the task of interpreting the questions to survey takers and they may get it wrong at times.
For example, in a recent conversation I had at a national conference with a Program Director of a military-based program, I learned that, despite his best efforts, trainees often interpret “service” in questions related to the “Appropriate balance between education and patient care” item as their military service, and automatically respond that service takes precedent, leading to citations.
The 2023 ACGME survey window closed on April 9, 2023, and all 118 programs in our institution scheduled to take the survey reached the required 70% completion rate, thanks to the participants’ efforts. We are grateful to all of you who participated in the 2023 ACGME survey. Your valuable feedback enables us to improve the overall clinical learning environment in our institution. Thanks to you we can identify struggling programs and offer support through the Special Review process. Through which we have been able to advocate and obtain more Advanced Practice Providers (APPs) for services in need, address issues of faculty professionalism, enhance resources such as sleep and lactation facilities, and much more. Thanks to you, we can also identify institutional trends that we need to work on. A good example is the recent launch of the “Prioritizing Ourselves When Fatigued” refresher, an eLearning module we created in response to scoring below our expectations on the item “Instruction on minimizing effects of sleep deprivation”.
On the flip side of all of this, when the survey goes unfilled, it leaves the ACGME without the necessary data to make decisions, leading to extended citations, issuing of new citations, and denying program expansion requests.
As you consider your feedback and review this year’s survey results, keep in mind the following ways in which you can help improve your program and the quality of our learning environment:
- Take the ACGME survey every year. Your feedback is crucial!
- Advocate for change in your program. If you identify areas that need improvement, share your concerns with your program director, other leaders in your program or UW GME through our Report a Concern
- Get involved in your program’s quality improvement efforts. All programs are required to conduct an annual program evaluation. Get involved and help to make your program the best it can be.
Thank you for your commitment to the continuous improvement of graduate medical education. The data suggest we could not do it without you!
by amande | Apr 21, 2023 | Announcements, Events, GME News & Notes, News

Dear GME Community,

Cindy Hamra Associate Dean, GME
Opening April’s News & Notes as I try to do, with some reasons to celebrate. First, our programs and departments are celebrating our match results, and we are excited to welcome our new trainees to UWSOM this summer. We also note that April is National Arab American Heritage Month, another opportunity recognize the diverse members of our community.
In the GME Office, we’re excited to welcome two new team members: Chris Gibson has joined the GME Accreditation team as our new Affiliations and Agreements Specialist and Amy Wheat joins the Wellness team in an interim capacity as a new counselor. More information is below.
We are also excited about the news that Dr. Santiago Neme has accepted the position of UWMC-ML Medical Director. Dr. Neme completed his Internal Medicine residency, Infectious Diseases Fellowship and Master’s in Public Health here at UWSOM. He will step in for Dr. Tom Staiger, who is retiring. Both are really wonderful colleagues and true advocates for our trainees.
April’s News & Notes is full of events, reminders and resources.
Thanks,
Cindy

Policies and Processes
- Programs that have matched or extended an offer to a trainee who requires a disability accommodation, should reach out to the GME Office (Bre Smith) as soon as possible so that we can work with the Disability Services Office to support the program and trainee through the process.
- The UW Medicine Bias Reporting Tool is for sharing incidents of bias including racism, sexism, ableism, discrimination of any form or other behaviors that do not reflect the prioritization of inclusion and equity expected in all areas of our community.
- Additionally, the GME Concern Reporting tool is available to any members of the GME community to report concerns about the learning environment.
- Interpreter Services and the Office of Healthcare Equity have created an online guide dedicated to providing resources for accessing medical interpreters, tips for partnering with medical interpreters, reminders about laws and regulations and directions on what to do in emergencies. Please read more about Clear Communication: Every Patient, Every Time.
- The University of Washington continues to require facemasks in healthcare and clinical facilities after the statewide healthcare mask order from the Washington State Secretary of Health ends on April 3, 2023. This decision is in alignment with UW Medicine’s medical facilities, our public health partners and other local health systems.
- The GMEC has approved appointment of the following new program directors; ACGME appointments require Review Committee (RC) confirmation:
- Meena Ramchandani, Infectious Disease fellowship
- Nelson Chiu, Family Medicine Seattle & Family Medicine Chelan Track residencies (interim)
- Paul Swanson, Surgical Pathology fellowship (interim)
- Yongjun Liu, Gastrointestinal and Hepatic Pathology fellowship (interim)
- Jose Garcia, Advanced Geriatric Medicine fellowship
- Betty Zhang, Advanced Pediatric Inflammatory Bowel Disease fellowship
- Claire Sandstrom, Emergency Radiology fellowship
- The ACGME has a weekly e-Communication. If you wish to receive it, email ACGMECommunications@acgme.org.
Events of Interest
- Upcoming GME Lunch & Learns
- April 20: GMEPAC Process for AY25; recording and slides now available
- May 18: Final Evaluations & Training Verifications + GME Strategic Plan
- June 15: Cancelled; Please join us again on July 20th
- This year’s Scheduling Workshop will be taking on a new format! Join Allison Shults to refresh and enhance your MedHub scheduling skills as you prep for the upcoming academic year. Three optional sessions will be held to provide PAs and PDs the flexibility to tailor your attendance to suit your current comfort level – attend them all or pick and choose:
- Scheduling 101: May 2nd | 10:00am – 11:30am: This session covers scheduling fundaments, including an overview of billing guidelines & FTE, using the New Schedule Task Wizard to create your schedule for the upcoming academic year, creating and editing a service/activity, and creating and assigning shifts/calls.
- Scheduling 102: May 3rd | 10:00am – 11:00am: Attend this session to learn how you can leverage the Conference Import Wizard, create conferences from scratch, and create and assign continuity clinics.
- Scheduling 103: May 4th | 10:00am – 11:00am: During this session we’ll discuss managing and approving absences and leave requests within MedHub, as well as some of the MedHub reports that will help your schedule management: the Resident Scheduling Errors, Resident Absence Details, and Billing vs Budgeted report.
- RSVP is not required, and we hope to see many of you there! Please refer to the Save-the-Date email for Zoom links, or reach out to Allison at ashults@uw.edu with any questions.
- Housestaff Event: “You are not Broken: Cultivating Healthy Sexuality During Training.” 6:30-8:00pm on Thursday, May 18th All residents and fellows are encouraged to attend via Zoom. Registration is now open and will close on Tuesday, May 16th. Register today.
- Tim Dellit, Interim CEO, UW Medicine; Interim Executive Vice President for Medical Affairs; and Interim Dean of the School of Medicine, would like trainees to know that the School of Medicine is now beginning their listening sessions as the first step in the SOM strategic planning process. These sessions will be open forums for trainees to share their thoughts and will be led by consultants. There are several options available for different cohorts of the community as the group wants to hear the voices from all parts of our School of Medicine. The majority of these will be via Zoom to make participation easier. There will also be an opportunity for written input later in the spring and the group will be joining some standing meetings (e.g., NURF, CMFA) to gather input. See email from April 29, 2023.
- Please join the annual UWNURF/HQSC Health Equity Conference via Zoom on Monday, May 8 from 7:00 – 8:00 PM PST. This year’s presentation is Improving Care of Unhoused Patients. Please register and share with others. All are invited to participate.
- Call To Action: Menstrual Product Donations – In honor of Women’s History Month, Dr. Sãdé Rodriguez and the Seattle Children’s GME office are partnering with Seattle Children’s Food Security program and Seattle Towers of Tampons & Pyramids of Pads (T2P2) to collect menstrual products for people who cannot afford them. Dr. Rodriguez is a pediatric resident at Seattle Children’s, and is invested in addressing this urgent equity gap for patients, families, and the community. Learn more about how you can donate on CHILD.
- Other GME Events can be found on our calendar.
Projects and Resources
 The GME Annual Program Timeline: Please review for important dates for April and May.
The GME Annual Program Timeline: Please review for important dates for April and May.- A reminder that residents and fellows can access CareLink, UW’s employee assistance program. UW CareLink is the employee assistance program provided for PEBB benefits-eligible UW employees, their dependents, and other household members. Initial services are provided at no cost, and the call is toll-free. UW CareLink is available nationwide 24 hours a day, 7 days a week.
- The Human Subjects Division is launching a pilot project to offer drop-in Zoom office hours to student/resident researchers in April and May 2023. Their office receives many IRB applications from a wide variety of UW students, and often find that students of all levels would benefit from additional support in navigating the IRB process from the beginning. Go to their HSD Office Hours webpage for the schedule and Zoom information.
- The UW Health Sciences Library has announced a new institutional license for Covidence, a popular online platform for evidence synthesis projects including systematic reviews, meta-analyses, and more. This new license is available to all UW faculty, staff, and students and is made possible in partnership with the UW Schools of Dentistry, Medicine, Nursing, Pharmacy, Public Health, and Social Work. From April 24-27 the UW Libraries is offering Research Data Management Planning, an asynchronous online workshop for UW community members engaged in research with data.
- As part of a new initiative at UWSOM called Virtual Bedside Concerts (VBC), we are looking to recruit volunteer musicians who are interested in performing virtual concerts for patients in the hospital. Any and all instruments are welcome, we just ask that you have a documented history of music training and feel comfortable playing music for and interacting with patients over zoom. There are no hourly requirements, you can sign up to perform as many or as few concerts as your schedule allows. Our only requirements are that volunteers attend a virtual orientation session and officially register with our designated hospital volunteer programs before getting started. If you are interested or have any questions, feel free to reach out to vbcorg@uw.edu.
- Submit your 55 word story! When the pandemic began, two faculty members, Molly Jackson and Andrea Kalus, launched a 55-word story campaign in collaboration with the Well-Being team to capture the emotions and feelings of the moment through short vignettes. As a way of marking this moment, of three years with COVID-19 in our lives, UW Medicine Well-Being invites you to reflect on where you have been and where you are now through the creation of your own 55-word story. Share your three-year reflections in 55 words (or less) with our community here.
- Trainees are encouraged to subscribe to UW Medicine STAT|INFO ADVISORY which has been designed to disseminate official information via text message to keep the UW Medicine workforce informed during emergencies and situations that might disrupt normal operations.
- Set your pronouns in Identity.UW: You can now display your pronouns in UW systems such as MyUW, Zoom and soon Canvas and MyUW class lists when you click “Set pronouns” in Identity.UW.
- A new opt-in module, Prioritizing Ourselves When Fatigued is a 5 minute training intended as a brief reminder on the important issue of fatigue. Learning Gateway is happy to answer any questions about the module.
- Our new Leave of Absence webpage is now live on the GME website. Here you will find LOA planning information and resources along with an intake form to contact GME for leave planning assistance: Leave Planning Submission Form. This form can be completed by trainees or program leadership. The December 2022 Lunch & Learn on ‘Leave Policy and Guidelines’ provides an overview of both these new resources; please the recording and slides.
People
- Emergency Medicine residents are featured in UW EM Residents Team Up with UW Law Students for Novel Medicolegal Workshop.
- Axel Adams, Emergency Medicine R4, received the Resident Academic Achievement Award from the Council of Residency Directors in Emergency Medicine.
- Alwiya Ahmed, Internal Medicine resident, is lead author and Matthew Triplette, associate professor, Pulmonary, Critical Care and Sleep Medicine, is senior author of “Delays in Recommended Follow-up after Positive Findings in Lung Cancer Screening” in the Annals of the American Thoracic Society. Department of Medicine co-author is Kristina Crothers.
- Maheetha Bharadwaj, Urology resident, is featured in ‘Volunteer-Led Virtual Bedside Concert Program Thrives’ in The Huddle.
- Joey Chiang, internal medicine resident,, is co-author of “Population-Level Health Effects of Involuntary Displacement of People Experiencing Unsheltered Homelessness Who Inject Drugs in US Cities” in JAMA.
- Fiona Gallahue, Emergency Medicine Residency Program Director, received the Michael P. Wainscott Program Director Award from the Council of Residency Directors in Emergency Medicine.
- Chris Gibson has joined the GME Office as our new Affiliations and Agreements Specialist as of March 20, 2023. Chris joins our team after serving as a Research Manager at Ducharme, McMillen & Associates. During his tenure, he oversaw compliance matters that spanned multiple jurisdictions, led a team of research analysts, provided mentorship and training to team members, and managed an online platform and information database for managing international tax matters. Additionally, Chris recently earned a Master of Public Health degree.
- Fuki Hisama, Medical Genetics and Genomics Program Director, has been elected to serve on the Board of Directors of the American College of Medical Genetics and Genomics (ACMG) for a six-year term. She has served on the board of directors of the American Board of Medical Genetics and Genomics (ABMGG), the Program Committee of the American College of Medical Genetics and Genomics, and the Medical Genetics Residency Review Committee of the Accreditation Council of Graduate Medical Education.
- Ellora Karmarkar, Infectious Diseases fellow, is quoted in “Deadly fungus spreading in U.S. with approximately 60% mortality” in MyNorthwest.
- Hannah Linden, Hematology and Oncology Fellowship Associate Program Director, is lead author of “Can Molecular Imaging Find a Path to Navigate Evolving Breast Cancer Treatments?” in Clinical Cancer Research.
- Manoj Menon, Hematology and Oncology Program Director, has been appointed holder of the Scripps Endowed Professorship in Hematology..
- Somnath Mookherjee, Academic Hospitalist Fellowship Program Director, is the 2023 recipient of the Society of Hospital Medicine Excellence in Teaching Award, which recognizes outstanding teaching prowess and mentoring to other hospitalists, residents, medical students, or other healthcare professionals.
- Santiago Neme has accepted the position of UWMC Medical Director. Neme is a dedicated, collaborative leader, who champions change. He is a very talented clinical faculty member who is well positioned to lead us through the health care challenges we face today. Dr. Neme’s appointment will begin July 1st, 2023. Please join us in congratulating Dr. Neme.
- Anzela Niraula, Endocrinology fellow, is lead author, and Joshua Thaler, associate professor, Metabolism, Endocrinology and Nutrition, is senior author of “Prostaglandin PGE2 Receptor EP4 Regulates Microglial Phagocytosis and Increases Susceptibility to Diet-Induced Obesity” in Diabetes. Department of Medicine co-authors are Kelly Ness, Jeremy Frey, Sophia Cuschieri, and Mauricio Dorfman.
- Robin Stiller, Pulmonary, Critical Care and Sleep Medicine fellow, is lead author and Tyler Albert, associate professor (General Internal Medicine) is senior author of “Responsibilities of Internal Medicine Chief Residents in the Modern Era: A National Survey” in ATS Scholar. Department of Medicine co-authors are Gabrielle Berger, Başak Çoruh, and Paul Cornia.
- Aiming to better predict who is at greatest risk for checkpoint inhibitor-induced hepatitis, Erica Storm, internal medicine resident, and colleagues conducted a retrospective case-control study of adults who newly received checkpoint inhibitor therapies for a variety of solid organ malignancies between 2016 and 2020 at Fred Hutchinson Cancer Center. Storm identified 97 cases of Grade 2-4 immune-related hepatitis. After adjusting for other factors that could contribute to risk of hepatitis, a liver cirrhosis was found to be associated with lower risk of immune-related hepatitis. In contrast, the presence of cancer metastases within the liver was associated with higher risk. Learn more on the Internal Medicine residency website.
- Joshua Thaler, Associate Program Director for Metabolism, Endocrinology and Nutrition fellowship, is quoted in “Is Antihistamine Use Making Me Gain Weight?” from The Huddle.
- Amy Wheat joins the GME Wellness team this month as a new, interim wellness counselor. Amy brings her unique perspective as a therapist, as well as her life experience of being partnered with a physician. Read more about Amy here. Trainees can make appointments with Amy on Schedulicity.
- Bessie Young, Vice Dean of Equity, Diversity, and Inclusion for UWSOM, is quoted in “Celebrating (But Not Touching) Black Women’s Hair” in The Huddle.
by amande | Apr 7, 2023 | Announcements, News

Byron Joyner, MD, MPA
This month, we celebrate the incoming class of trainees who will join us this summer! For the third year in a row, our residency and fellowship programs virtually recruited the best and the brightest medical students from around the country – and the world! This year, 84 of our 200+ total ACGME and non-ACGME training programs participated in the National Residency Matching Program (NRMP) and 23 participated in the San Francisco Match.
Both the NRMP Main Residency and Specialties Matches were the largest on record, with 40,375 positions available in the Main Residency Match and 13,365 positions in the Specialties Match. This year was also our largest Match at UWSOM with 299 positions offered in the Main match and 191 in the Specialties Match.
Main Residency Match
- In the Main Residency Match, the 26 participating UWSOM residency programs had a match rate of 98.7% (and 99.3% after the Supplemental Offer and Acceptance Program, or SOAP) compared to 93.3% nationally.
- From 2019-2022 we saw small year-to-year decreases in the number of UWSOM graduates matching to our residency programs. This year, we matched 56 UWSOM graduates (an increase of 17 from 2022) or 19% of our matched applicants.
- Nationally, the number of matched US MD seniors, US DO seniors, US citizen IMGs, and non-US citizen IMGs increased from last year. The number of unmatched US MD seniors to PGY-1 positions decreased again this year, a two-year trend.

Specialties Matching Program
- In the Specialties (fellowship) Match, the 58 participating UWSOM fellowship programs offered 191 positions with a match rate of 91.6% compared to 86.4% nationally. Another 10 positions have been filled post-Match.
- 41 of the 175 spots filled in the Match were filled by UWSOM residents, a slight decrease from 2022.
- Nationally, the number of matched UW MD graduates, US DO graduates, US citizen IMGs, and non-US citizen IMGs increased from last year.
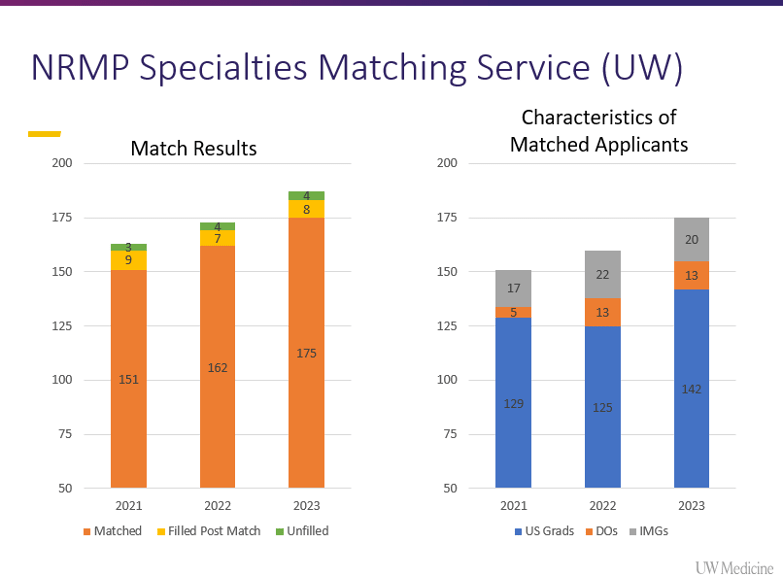
The past three years have been difficult, but UWSOM programs continue to have strong match results and we remain a very competitive training institution, as reflected by the 5-year trends below:

Increasing Diversity in our Training Programs
UW Medicine is creating a healthcare system that works for everyone. To that end, it is essential that we prioritize diversifying the medical workforce. This is not just a moral imperative. It is a practical one, as diversity can lead to better health outcomes and a more effective healthcare system overall.
This year our programs reported increases in both Black, Indigenous and People of Color (BIPOC), as well as Underrepresented in Medicine (URM) candidates who matched in our medical and dental programs. As we work together to increase and, more importantly, sustain inclusivity and diversity in our workforce, we can continue to provide better equity of patient care in our community.
I want to congratulate program and department leadership, residents and fellows, and the Network of Underrepresented Residents and Fellows (NURF) for their tremendous efforts in our journey to diversify our learning community. For the third year, the GME Office and NURF hosted Town Halls to help our programs attract underrepresented and vulnerable minority candidates. One of the NURF Town Halls had more than 600 participants.
Below is this year’s representation of BIPOC, URM and women who have historically been minoritized in Medicine, as reported by our departments.
| Department |
BIPOC |
URM |
Women |
| Anesthesiology & Pain Medicine |
39.0% |
7.0% |
14.0% |
| Orthopaedics & Sports Medicine |
12.5% |
25.0% |
25.0% |
| Family Medicine |
60.0% |
20.0% |
60.0% |
| Laboratory Medicine and Pathology |
9.56% |
8.82% |
52.41% |
| Medicine |
41.8% |
15.4% |
42.4% |
| Obstetrics & Gynecology |
85.0% |
42.0% |
100.0% |
| Ophthalmology |
80.0% |
20.0% |
40.0% |
| Otolaryngology |
75.0% |
25.0% |
0.0% |
| Pediatrics |
51.0% |
15.0% |
68.0% |
| Physical Medicine and Rehabilitation |
0.0% |
9.0% |
36.0% |
| Psychiatry & Behavioral Sciences |
33.5% |
6.0% |
64.2% |
| Surgery |
44.0% |
19.0% |
88.0% |
| Urology |
25.0% |
25.0% |
100.0% |
*See 2022 results and 2021 results
All members of our community, including the department chairs, residents and fellows, program directors and administrators, faculty, and staff, worked together to produce these excellent results. Especially during these challenging times, it is critical that we cultivate an environment where everyone feels safe and as though they belong, an environment in which everyone can be successful.
Congratulations and thank you!
Byron Joyner, MD, MPA
Vice Dean for GME and DIO
by amande | Mar 24, 2023 | Announcements, Events, GME News & Notes, News

Dear GME Community,

Cindy Hamra Associate Dean, GME
This month brings lots of great celebrations – first, last Friday was Match Day. It’s been fun to talk with programs and hear their excitement about our matched residents and fellows. We look forward to onboarding and welcoming them to the University of Washington!
In the GME Office, we welcome two new team members. Bethany Griffitts is our new Fiscal Specialist on the Finance Team and Chris Gibson is the new Affiliations and Agreements Specialist on the Accreditation Team. If you’re not sure who to contact about a GME related question, check out the Our Team page.
A few other notes and reminders. Ramadan started on March 22 – the Info by Training Site page includes information about prayer / meditation spaces and other resources. Spring is also the time when UW’s cherry blossoms begin to bloom. Finally, March is Women’s History Month – check out this article by UW Medicine’s Office of Healthcare Equity featuring lesser known healthcare sector pioneers and this article in UW Huddle where women share their experiences in male-dominated fields.
Thanks,
Cindy
Policies and Processes
- The GMEC approved revisions to the following policies at the March meeting. All are posted on the Policies and Procedures page of the GME website.
- Annual Program Evaluation: Revisions include alignment with the upcoming changes to the ACGME’s Common Program requirements (CPRs) scheduled to take effect in July 2023; addition of a Purpose statement; process section updated to reflect the new language that requires a review of outcomes from prior APEs, program evaluations by trainees and faculty, and allows flexibility in the data elements reviewed; added that tracking Workforce diversity also needs to include staff and community members; and added Equity, Diversity, and Inclusion to CLER questions
- Eligibility and Selection Policy: Revisions include minor changes to reflect new CPRs effective July 2023; under Program Policies, grouped requirements as specialty-specific and UW specific and moved selective service and NIH grant restrictions up from footnote; moved footnote addressing program communication to applicants of changes to salary and benefits with grant funding up into Interview and Selection section.
- Visa Policy: Revisions include updating Scope to apply to programs (not trainees) and changed non-accredited training programs to ACGME Non-Standard Training (NST) Programs. Amended footnote to include definition of an NST program; added Purpose statement to align with format of other GME policies; and updated J-1 section to reflect changes under new ACGME NST requirements
- Programs that have matched or extended an offer to a trainee who requires a disability accommodation, should reach out to the GME Office (Bre Smith) as soon as possible so that we can work with the Disability Services Office to support both the program and trainee through the process.
- Due to decreasing COVID case counts and hospitalizations, effective Tuesday, March 7th the UW Medicine Required and Extended-use Mask Policy was updated with the following changes:
- Respirators are no longer required for all aerosol generating procedures. Respirators continue to be strongly recommended, in addition to other personal protective equipment (PPE), to prevent the acquisition and transmission of COVID and other respiratory viruses during these procedures. Respirators, in addition to other PPE, continue to be required for the care of all patients with known or suspected COVID-19. Respirators will continue to be provided to all staff who choose to use them.
- Physical distancing and masking are no longer required in breakrooms, team rooms, multi-person offices, conference rooms, and similar rooms isolated from patient care spaces by a door or away from patient care spaces. Using a mask or respirator in those spaces continues to be strongly recommended.
- Masks or respirators continue to be required in all patient care spaces, public spaces ( hallways, elevators, and cafeterias), and during all patient care and visitor interactions. Please ensure you have a mask or respirator on when entering and leaving patient care buildings. Masks may also be required by Employee Health following a high-risk exposure or recent COVID-19 infection.All healthcare workers should continue to wear the highest level of respiratory protection that they can tolerate as they may encounter people with asymptomatic COVID or other respiratory infections. Wearing a mask or respirator also protects those around you in case of asymptomatic or pre-symptomatic COVID infection.
- Welcome New Program Administrators:
- Lanie Cueva, Pediatric Hematology-Oncology
- Taraneh Moll, Clinical Informatics
- Keely Peddycord, Child Neurology
- The GMEC has approved appointment of the following new program directors; ACGME appointments require Review Committee (RC) confirmation:
- Rebecca Petersen, General Surgery Residency
- Ari Pollack, Pediatric Nephrology Fellowship
- Christopher Burke, Advanced Cardiac Surgery Fellowship [Non-ACGME]
- Rebecca Ronsley, Pediatric Neuro-Oncology Fellowshipb [Non-ACGME]
- The ACGME has a weekly e-Communication. If you wish to receive it, email ACGMECommunications@acgme.org.
Events of Interest
- Upcoming GME Lunch & Learns
- March 16: Annual Program Evaluations; recording and slides now available
- April 20: GMEPAC Process for AY25
- May 18: Final Evaluations & Training Verifications + Additional Topics
- GME Onboarding Drop-in Session: For additional support for program administrators, please find below a schedule for the upcoming informational drop-in session. This is designed to help programs with our various onboarding processes and answer any questions, in a casual and virtual format.
- GME Onboarding Drop-in Session #2
- Date: Wednesday, March 29
- Time: 9-10am
- Zoom
- RSVP: Not required
- Tentative Talking Points include: Guided instruction on MedHub functions (Adding, Advancing, Terminating/Graduating); Onboarding packages (How to monitor resident and fellow status); What’s on the horizon for April and beyond; and time for Q&A.
- Cherry Blossom run/walk celebration at UW – March 25th (5k run/walk) and 26th (half-marathon). Space limited – register soon! See full calendar of events: Cherry Blossom Activities at the Burke! The cherry blossoms at the UW campus are a seasonal tradition and celebration for the entire region. This year’s colder-than-usual spring is demanding a little more patience. Mark your calendars for a peak bloom expected in early April.
- GME Outreach Event for trainees at SCH on April 14th from 11 am to 1 pm. We encourage trainees to stop by to say hello, meet our GME team members and take a packed lunch. Please look for an email closer to the event with specific room details.
- Other GME Events can be found on our calendar.
Projects and Resources
 The GME Annual Program Timeline: Please review for important dates for March and April.
The GME Annual Program Timeline: Please review for important dates for March and April.- The UW Professional Staff Organization (PSO) has launched the new Diversity, Equity, Inclusion and Belonging Excellence Award which seeks to highlight professional staff currently working at the UW. Nominees include those who have demonstrated a deep commitment to the advancement of Diversity, Equity, Inclusion and Belonging work directly within the UW and/or their local communities. Nominations are due April 15.
- The January 2023 DIO Blog featuring the work of the Care of Patients Experiencing Incarceration (CPEI) Task Force and Learning Gateway has been updated with the new Caring for Patients Experiencing Incarceration guide.
- Submit your 55 word story! When the pandemic began, two faculty members, Molly Jackson and Andrea Kalus, launched a 55-word story campaign in collaboration with the Well-Being team to capture the emotions and feelings of the moment through short vignettes. As a way of marking this moment, of three years with COVID-19 in our lives, UW Medicine Well-Being invites you to reflect on where you have been and where you are now through the creation of your own 55-word story. Share your three-year reflections in 55 words (or less) with our community here.
- The Health Equity, Advocacy, and Anti-Racism (HEAAR) Curriculum for the Internal Medicine Residency Program has been introduced by Drs. Lynsey Bernfeld, Hasib Yousufzai, Anna Morenz, Ryan Abe, Helen Jack and Anders Chen. HEAAR is a comprehensive, multi-tiered, and inter-professional curricular thread embedded into the residency program with the goal of learning principles of anti-oppression and using those frameworks to understand and address the structural origins of health inequities. Learn more on the Department of Medicine news site.
- Dr. Jennifer Best, Associate Dean of GME, wishes to highlight Dr. Carrie Cunnigham’s deeply personal and important President’s Address at the AAS Academic Surgical Congress. In the 45 minute video, Dr. Cunningham discusses the mental health crisis impacting our community, reflecting on her lived experiences. Dr. Best notes that, “it’s a message I think all of us need to hear.”
- Trainees are encouraged to subscribe to UW Medicine STAT|INFO ADVISORY which has been designed to disseminate official information via text message to keep the UW Medicine workforce informed during emergencies and situations that might disrupt normal operations.
- Set your pronouns in Identity.UW: You can now display your pronouns in UW systems such as MyUW, Zoom and soon Canvas and MyUW class lists when you click “Set pronouns” in Identity.UW.
- A new opt-in module from Learning Gateway is now available. Prioritizing Ourselves When Fatigued is a 5 minute module intended as a brief reminder on the important issue of fatigue. Learning Gateway is happy to answer any questions about the module.
- Our new Leave of Absence webpage is now live on the GME website. Here you will find LOA planning information and resources along with an intake form to contact GME for leave planning assistance: Leave Planning Submission Form. This form can be completed by trainees or program leadership. The December 2022 Lunch & Learn on ‘Leave Policy and Guidelines’ provides an overview of both these new resources; please review the recording and slides.
People
- Toni Brassfield, Resident, Internal Medicine, won top clinical vignette at the recent Northwest Regional Society for General Internal Medicine (SGIM) conference for his poster, “Strongyloides stercoralis hyperinfection following initiation of CHOP therapy”
- Debra Cherry, Program Director, Occupational and Environmental Medicine and John Scott, professor (Allergy and Infectious Diseases) talked to KIRO 7 News in “Safeguarding wearable technology.”
- John Choe, Associate Program Director, Internal Medicine, is co-author of “AAIM Recommendations for Undergraduate Medical Education to Graduate Medical Education Transition Curricula in Internal Medicine” in the American Journal of Medicine.
- Anna Condella, fellow, Pulmonary, Critical Care and Sleep Medicine, is lead author of “Veno-venous Extracorporeal Membrane Oxygenation for COVID-19: A Call For System-Wide Checks to Ensure Equitable Delivery For All” in ASAIO Journal. DOM co-author is Andrew Luks, Program Director, Critical Care Medicine.
- Shani Delaney, Program Director, Maternal-Fetal Medicine, is featured in UW study shows race-based prenatal test is outdated, ineffective – KREM.
- Mackenzie Holmberg, R3, Internal Medicine is lead author and Sarah Sanghavi, clinical assistant professor (Nephrology) is senior author of “Bridging the Gap: A Practical Approach to Discussing eGFR and Race with Medical Students” in the Clinical Journal of the American Society of Nephrology. DOM co-author is Başak Çoruh, Program Director, Pulmonary Critical Care.
- Nicholas Johnson, Associate Program Director, Critical Care Medicine, is co-author of “Total and subgenomic RNA viral load in patients infected with SARS-CoV-2 Alpha, Delta, and Omicron variants” in the Journal of Infectious Diseases.
- Vishesh Kapur, Program Director, Sleep Medicine Program, is quoted in “Here’s What Your Body Is Trying To Tell You If You’re Constantly Waking Up Before Your Alarm” in Well+Good.
- Eileen Klein, professor (Pediatrics) is one of this year’s recipients of the School of Medicine Excellence in Mentoring Women Faculty Award. Awardees are chosen based on recommendations from peers and mentees received by the Dean’s Standing Committee for Women in Medicine and Science.
- William Lombardi, Program Director, High-risk Coronary Intervention (CHIP) Fellowship, is the 2023 recipient of the TCT Geoffrey O. Hartzler Master Operator Award. He is receiving this award for his superior operator skills and leadership in interventional cardiovascular medicine.
- Leo Morales, professor (General Internal Medicine) is quoted in “University of Washington study will survey Latinos in the state with COVID-19” and “WA Hispanics suffer high rates of long COVID. UW study launched to find out more” in the Yakima Herald-Republic. He is also featured in Long COVID in WA Hispanics being studied — high rates expected from the Bellingham Herald.
- It is with great pleasure that the Department of Family Medicine announces the hiring of Joseph Nelson as the inaugural Associate Program Director for Diversity Equity and Inclusion for the residency. Joey is a member of the Confederated Tribes and Bands of the Yakama Nation. He is a graduate of the UW School of Medicine and the UW Family Medicine Residency and practices broad spectrum family medicine. During his time as a resident he was a leader in our Health Equity and Anti Racism (HEAR) Committee and the President of the Network for Underrepresented Residents and Fellows (NURF). Joey currently serves as the Academic Chief Resident where he applies his unending positive energy to the advancement of the HEAR vision, the betterment of the residency and the UW Department of Family Medicine.
- Urology resident Chloe Peters is first author of “Pregnancy and parental leave in medicine and academia — a focus on urology” in Nature.
- From the UW Medicine Newsroom: Medical students meet their matches
- Check out the UW Otolaryngology-HNS Winter 2023 Newsletter for lots of great faculty and trainee highlights.
by amande | Mar 10, 2023 | Announcements, News
-
-
 Jennifer Best, MD |
 Cindy Hamra JD, MA |
 Byron Joyner, MD, MPA |
|
|
Exciting times are afoot within the GME Office!
Now to be fair, our team finds all the work we do exciting, but at this moment we are working to finalize our GME Strategic Plan for AY2024 to 2029. In this edition of the Blog, we would like to provide our community with an overview of work to date and what you might expect moving forward.
How Our Community Has Informed The Process
You may recall that in July 2022, we sent a survey to our community and stakeholders, including our residents and fellows, program directors and administrators, department administrators, chairs, and leaders of UW Medicine. Our goal here was to “broaden the circle” of voices, as compared with previous iterations of strategic planning. We appreciated hearing from many of you within the context of this SWOT (Strengths / Weaknesses / Opportunities / Threats) analysis about the work we accomplished related to our prior strategic plan and where there is work still to do.
How We Analyzed The Data
A group of GME team members sat with those results to identify themes for each group of stakeholders, with specific attention to themes identified by multiple groups as important priorities. Knowing that our work must be aligned with broader systems, the second step involved evaluated mapping this narrower list of themes against “inputs” that we felt would raise their priority moving forward, including UW Medicine strategy, our Equity Blueprint, ACGME requirements, and our own sense of emerging priority areas that has evolved as we engage each day with individuals, programs, and departments.
Emergent Priority Areas
Our previous strategic plan was predicated on list of key values that drove our work. Because we believe this has been an effective way to share our goals internally and externally, we will be communicating our new strategic plan on these same Strategic Values. At a high level, the following areas have emerged as key for AY24-29
ADVOCACY
Does everyone in our community have what they need to do their jobs and feel valued? How do we help programs avoid accreditation threats? Can GME fund the work it wants to do?
COMMUNICATION
Do members of the GME community feel connected with one another? Do we learn from one another and avoid reinventing the wheel?
EXPERTISE
How do we create standards where they haven’t existed before? How do maximize our use of technology? How can we come to be seen as the standard for GME?
INTEGRATION
How do we help programs to anticipate and respond to the shifts in clinical needs? How do we do more with limited resources? How do we support UW Medicine’s goals of serving the region?
PEOPLE
How do we bring, grow, and keep the right people, doing the right work? How do we create an environment in which all members can reach full potential? How do we heal and care for our community?
QUALITY AND VALUE
Can we be more strategic in data collection and reporting? How do we effectively “speak the language” of decision-makers when advocating for resources? How can we raise the visibility of learning environment needs that are common across programs and departments?
What’s Next?
We are vetting a draft of the Strategic Plan within the GME Office, including careful thought about how we will know we are making progress (What are our key performance indicators and outcomes?) We plan to bring a draft back to some members of the broader community that identified a desire to participate in a focus group with the plan to present the plan to the Graduate Medical Education Committed (GMEC) and share the final plan more broadly with our stakeholders – including you – in May and June.
This is important work – work that will take all of us. The worlds of clinical care, health professions education and GME are complex, and always shifting, as is the world around us. Thank you for the privilege of working on your behalf as your partners in this next season.
- Jennifer Best, MD
Associate Dean, Accreditation and Education
- Cindy Hamra, JD
Associate Dean, Operations and Administration
-
- Byron Joyner, MD, MPA
Vice Dean for GME and DIO
by amande | Feb 24, 2023 | Announcements, News

On this Thank A Resident Day, the UW GME team wishes to express our wholehearted gratitude for the many ways that residents and fellows enhance our community by bringing their best to challenging circumstances, supporting one another and working diligently to learn, grow and inspire change.
Yet there may be no better way, perhaps, to honor our trainees’ impact than by sharing the words of patients whose lives they improve each day. For these individuals, the work of residents and fellows is never unnoticed. These are just some of the recent comments received by UW Medicine. It is a privilege to receive and share them.
The resident helping me is a rockstar – very warm, helpful, informative, comforting and insightful.
I could have seen someone else saying, “You’ll need another appt. for all this.” But she dived in and got it done.
I would like to switch to this doctor because he is absolutely fantastic and knows what he is doing. Very well educated, concerned about everything you have to say and makes sure everything is done properly and you feel good about the visit with him.
…kind, gentle, attentive, and the model of excellent primary care
…talked to me with respect, not down to me. Several doctors and nurses treated me as an old woman and didn’t know or understand. I am an old lady but I am not senile. I still have all my marbles.
I loved that I had a female surgeon. She was knowledgeable, confident and caring.
A wonderful doctor- knowledgeable, caring, empathetic, and informative…I GREATLY appreciate her respectful “partnership approach” to my healthcare.
Always there for me. I love the professional manner in which he handles medical concerns.
She also told me she was here for me if I needed anything. I really appreciated that.
The resident on my case made my experience better.
Education can at times feel somewhat abstract, yet we are fortunate that in health professions education, relationships with patients are protective and centering. The moments represented above are anything but abstract. They are vulnerable, deeply interpersonal and filled with shared optimism. And today, we celebrate that they are only made possible by the exceptional personal qualities and commitment of our residents and fellows.
From those of us who work alongside you in hospitals and clinics, and the team of staff that make that clinical and educational work possible, thank you for inspiring our hope in the future of healthcare!
Jennifer Best, MD
Associate Dean, Accreditation and Education
Cindy Hamra, JD
Associate Dean, Operations and Administration
Byron Joyner, MD, MPA
Vice Dean for GME and DIO

by amande | Feb 23, 2023 | Announcements, Events, GME News & Notes, News

Dear GME Community,

Cindy Hamra Associate Dean, GME
February is Black History Month – there are so many good resources available, and I enjoyed reading President Cauce’s blog and the UW Combined Fund Drive’s engagement and learning opportunities. As we work to support our community, a reminder that Ramadan begins on March 22. Muslim colleagues and patients may be fasting between dawn and sunset in observance.
Additional celebrations in February include Thank a Resident Day on February 24. This day is an opportunity to recognize our trainees and their enormous contribution to our mission. In the spirit of celebrating our trainees, GME enjoyed partnering with The Huddle to craft this Getting to know our Chief Residents and Fellows article.
Finally, we are excited to welcome Allison Shults to the GME team as RMS and Information Systems Manager. In this role, Allison will be our MedHub subject matter expert and will lead a new strategic initiative to prioritize use of data in our work in GME. Allison joins us from the Foster School of Business at the University of Washington, where she was previously Assistant Director in the Master of Science in Information Systems program.
Thanks,
Cindy
- The GMEC has approved appointment of the following new program directors; ACGME appointments require Review Committee (RC) confirmation:
- Anshu Bandhlish, Cardiovascular Pathology (Interim)
- Matthew Cham, Cardiothoracic Imaging
- Amanda Kost, Family Medicine – Medical Education Research
- At its January meeting, the ACGME granted Initial Accreditation to a new Internal Medicine residency program based in the Department of Medicine. The UW-Alaska Internal Medicine Rural Residency Program’s mission is to provide an intensive Alaska-based, rural primary care-focused training experience in internal medicine. This is the very first accredited rural residency training program in Internal Medicine in the country. More information on the Department of Medicine news site and at the UW Medicine Newsroom
- The ACGME has a weekly e-Communication. If you wish to receive it, email ACGMECommunications@acgme.org.
Events of Interest
- Upcoming GME Lunch & Learns
- February 16: Workplace Safety; recording and slides now available
- March 16: Annual Program Evaluations
- April 20: GMEPAC Process for AY25
- For additional support for program administrators, please find below a schedule of *optional* informational drop-in sessions. The available drop-in sessions are designed to help programs with our various onboarding processes and answer any questions, in a casual and virtual format.
- GME Onboarding Drop-in Session #1
- Date: Tuesday, February 28
- Time: 9-10am
- Zoom
- RSVP: Not required
- Tentative Agenda:
- Guided instruction on MedHub functions
- Forms: one-step stipend increase, extensions, Job Profile Change/Program Transfer
- Q&A
- GME Onboarding Drop-in Session #2
- Date: Wednesday, March 29
- Time: 9-10am
- Zoom
- RSVP: Not required
- Tentative Agenda:
- Register for “Fertility & Family Planning for those in Medicine & Science.” The UW Committee on Women in Medicine & Science will be hosting this workshop on Thursday March, 2 from 4:00 – 5:00 PST. This workshop will be presented by Rachel M. Whynott, MD, FACOG, Assistant Professor & Associate Fellowship Director, Division of Reproductive Endocrinology and Infertility at the University of Washington. It will discuss planning for pregnancy, what fertility testing may be appropriate for individuals, when to see fertility assessment, and fertility preservation options. Zoom information will be sent within the week prior to the event to those registered. For those unable to attend, materials and a recording of the event will be posted to the website afterward.
- Other GME Events can be found on our calendar.
Projects and Resources
 The GME Annual Program Timeline has been updated and is now organized by activity type, eg ACGME Accreditation, Appointments and Onboarding, Program Activities, Recruitment. Please review the updated document and note the important dates for February and March.
The GME Annual Program Timeline has been updated and is now organized by activity type, eg ACGME Accreditation, Appointments and Onboarding, Program Activities, Recruitment. Please review the updated document and note the important dates for February and March.- Set your pronouns in Identity.UW: You can now display your pronouns in UW systems such as MyUW, Zoom and soon Canvas and MyUW class lists when you click “Set pronouns” in Identity.UW.
- 2024 ACGME Awards: Nomination materials are available on each award’s page in the Awards section of the ACGME website. All nominations are due March 15, 2023. Please reach out to the GME office if you plan to submit an application.
- UW Medicine launched an Equity, Diversity and Inclusion Survey to identify baseline measures of Equity, Diversity, and Inclusion across UW Medicine and provide actionable data to help prioritize areas for work at the entity and departmental levels. All UW Medicine faculty, staff, and trainees are invited to complete the survey which will take about 10-15 minutes to complete. The survey closes February 28, 2023. Please participate in this survey to help make us a more equitable and anti-racist institution.
- The NRMP will be holding an Introduction to the Fellowship Match webinar for NRMP Match participating specialties on Thursday, February 16, from 10:00 – 11:00 a.m. Learn about program staff roles and responsibilities, managing your program’s participation in the Match, ranking applicants, and important policy information. Advance registration is required.
- The GME Office is currently recruiting for an Affiliations and Agreements Specialist (req. 212955)
- Trainees are encouraged to subscribe to UW Medicine STAT|INFO ADVISORY which has been designed to disseminate official information via text message to keep the UW Medicine workforce informed during emergencies and situations that might disrupt normal operations.
- A new opt-in module from Learning Gateway is now available. Prioritizing Ourselves When Fatigued is a 5 minute module intended as a brief reminder on the important issue of fatigue. Learning Gateway is happy to answer any questions about the module.
- Our new Leave of Absence webpage is now live on the GME website. Here you will find LOA planning information and resources along with an intake form to contact GME for leave planning assistance: Leave Planning Submission Form. This form can be completed by trainees or program leadership. The December 2022 Lunch & Learn on ‘Leave Policy and Guidelines’ provides an overview of both these new resources; please review the recording and slides.
People
- Congrats to members of our GME community who were nominated for the 2022 – 2023 Distinguished Staff Awards.
- Geoffrey Baird, Chair, Laboratory Medicine and Pathology, is quoted in “Is it time for a reality check on rapid COVID tests?”.
- The U.S. Surgeon General, Vivek Murthy, took to social media to highlight the efforts of Justin Bullock, fellow, Nephrology, who advocates for greater mental health support for health workers.
- Fionnuala Cormack, clinical associate professor (Nephrology) will serve as the Associate Program Director for the Nephrology Fellowship Program, effective July 1, 2023. She brings tremendous strengths and experience to this role. She has served as the Director of the UW dialysis program, leads the Nephrology efforts at UW Stone Center, and is the Section Head of UWMC’s NW Campus. She is a gifted educator, and the fellows recognized her with the Teacher of the Year award for the 2019 – 2020 academic year.
- Tim Dellit, Interim Dean and CEO of UW Medicine, is quoted in “Gonzaga Law School, UW Medical ends participation with U.S. News rankings” – KXLY
- The Department of Surgery Newsletter ‘Surgery Synopsis’ features many voices of the GME community, including Program Directors, trainees, and program staff. Check out the Winter 2022 / 2023 issue.
- Yolanda Evans, alum, Adolescent Medicine Fellowship, is featured in The Huddle piece, “How alumna Yolanda Evans improves adolescent health by pausing and listening to youths’ needs”
- Roxanne Hicks, R3, Internal Medicine has been accepted into the Society of General Internal Medicine (SGIM) Leadership in Health Policy Program (LEAHP). The Leadership in Health Policy Program aims to develop SGIM members who are effective and active health policy advocates and local health policy experts, leaders, and teachers; to offer health policy career development resources and opportunities to all SGIM members; and to develop an expanding, national cadre of Health Policy Committee members and broaden engagement in the Society’s health policy efforts.
- Trish Kritek, professor (Pulmonary, Critical Care and Sleep Medicine) won the Reeves Prize for Presentation Excellence at the 2023 International Hypoxia Symposia in Lake Louise for her talk “Hypoxemia in the COVID ICU — Mechanisms and Reflections.”
- The University of Washington’s Latino Center for Health has launched a study to better understand the extent and impact of long COVID on the state’s Latino communities. “Since the onset of the pandemic, Latino communities in Washington state have had higher rates of COVID-19 infection than the general population, higher rates of hospitalization, and higher rates of mortality on an age-adjusted basis,” said Leo Morales, professor (General Internal Medicine) and co-director of the Latino Center for Health. “Yet we are not seeing many people from Latino communities showing up in our long-COVID clinics.” Read more from UW Medicine Newsroom.
- To improve HIV testing rates in the West African country of Côte d’Ivoire, community health workers need more training and support, researchers from the UW and the Institute de Recherche et Actions en Afrique, Abidjan, Côte d’Ivoire report in a new study. “We need to identify people who are infected if we are going to treat them, but identification can be the hardest of the three 95 percent goals to achieve,” said Nancy Mugisha, fellow, Allergy and Infectious Diseases, and lead author of the paper published in PLOS ONE. Read the full story from UW Medicine Newsroom.
- Henry Ou, Program Director, Pediatric Otolaryngology, is featured in Meet Henry Ou, a Pediatric Otolaryngologist at Seattle Children’s.
- Paul Pottinger, Program Director, Infectious Diseases, is quoted in “Too Many People Are Using Neti Pots and Vaporizers Unsafely, Survey Suggests” in Everyday Health.
- Sarah Prager, Program Director, Complex Family Planning, is featured in “In a post-Roe world, miscarriage treatment becomes more difficult.”
- Sarah Prager, Program Director, Complex Family Planning, is featured in “How a Texas ruling on abortion pills would affect Washington.”
- UW Medicine has announced the creation of a historic endowed deanship honoring retired Dean Paul G. Ramsey. The Paul G. Ramsey Endowed Deanship was established with leadership gifts from Steve and Connie Ballmer and the Bill & Melinda Gates Foundation. Each donated $10 million to advance research discoveries, train medical leaders and further excellence and equity in health care.
- Colbey Ricklefs, R3, Family Medicine, is leading an initiative to rid insurance codes of pejorative language.
- Grace Shih, Co-Director, Reproductive Health & Advocacy Fellowship, is quoted in “Post-Roe, vasectomies tick up in the Seattle area” – KUOW
by amande | Feb 8, 2023 | Announcements, News, Sticky

The chief residents and fellows at UW Medicine are key players in the clinical space through their guidance and leadership, but who are they?
The chief residents and fellows are trainees, usually senior, who serve as the leaders and representatives for the group of residents or fellows in their training program. Their roles and responsibilities can vary greatly depending on their program, but each chief resident and fellow is expected to be a model of professionalism, to communicate or liaise with a variety of stakeholders to represent their trainees’ needs or opinions, and to provide counsel to trainees about all matters — big or small.
These roles are essential at UW Medicine because these individuals represent the interests and opinions of a critical group of the workforce while also acting as subject matter experts. They answer questions that would otherwise go to faculty or administrative staff and bring knowledge and insight that might otherwise get lost when developing policies, practices and communications. Many chiefs eventually pursue faculty roles and become clinician educators within the system.
Serving as chief is also an opportunity for a trainee to expand their leadership skills and get insight into the complexities of how a training program is operated. The selection process varies depending on the program. Some programs hold faculty or peer elections, while others have faculty members select trainees based on written criteria. All chiefs are chosen for their leadership abilities, clinical or scholarly accomplishments, administrative or oversight abilities, and strong communication and interpersonal skills.
To be a chief resident or fellow is a prestigious honor — one that can involve an additional year of training beyond the board eligibility and requires a large amount of attention. It denotes a respected leader.
Get to know some of the chief residents and fellows >
by amande | Feb 6, 2023 | Announcements, News

Byron Joyner, MD, MPA
There are many symbols in our country that reflect the struggle of Black people in America.
For this month of Black History celebration, I choose to focus on The Embrace, the new controversial sculpture in the Boston Commons, unveiled just last month. It reminds me of the ultimate commandment – which is to love one other.
Of all the Civil Rights statues standing, it is one of few that commemorates both Martin Luther King, Jr. and his wife, Coretta Scott King. The 20-foot, 19-ton bronze sculpture was designed by Hank Willis Thomas, an African American artist who works primarily with themes related to identity, history and popular culture. The work was chosen from more than 200 entries in a competition by the Boston public. From the moment of its unveiling, The Embrace has been criticized in the press and social media and panned widely by critics for its stylistic ambiguity and suggestive imagery.
I have not seen the sculpture yet, but I’m compelled to write about it because of its intended meaning. The Embrace is a great symbol of an iconic man, Martin Luther King, Jr., sharing a tender moment with his wife after he won the 1964 Nobel Peace Prize.
Until that moment, the Nobel Peace Prize had only been awarded to two Black men: Ralph Johnson Bunche, a political scientist, diplomat and leading actor in the mid-20th Century decolonization process and the US Civil Rights Movement; and Albert John Luthuli, a Black South African and anti-Apartheid activist. At just 35-years old, Martin Luther King, Jr. was the youngest American ever to win the coveted prize for combatting racial injustice through non-violent resistance. Four years later, he was dead.
The Embrace represents the strong arms of MLK and is supposed to be the embodiment of a beloved community. We may not be there yet, but I have hope. Is it possible for us to think of what is good instead of demeaning the tremendous work of art and the artist? Especially now, at a moment that is so critical to our post-COVID-19 recovery, which has, in many ways, led to our isolation and desocialization, we need to think of King’s legacy as the reification of kindness.
King is arguably the most influential figure of the Civil Rights movement. This statue is a bold aide-mémoire that models for us what we should all be doing – and that is creating human touch and building up humanity, not tearing it down. There have been critical memes and statements debasing the statue, taking a swipe at our sacred and dignified man who shares a tender moment with his wife, an embrace displayed to the worldwide community at a time when we can all use a hug.
Take a moment out of your busy lives to embrace a friend, a family member, or a colleague during the month of February. We need less judgment and more love in our lives. In a world where we are taught, you can be anything, be kind.
Embrace The Embrace.
by amande | Jan 20, 2023 | Announcements, Events, GME News & Notes, News

Dear GME Community,

Cindy Hamra Associate Dean, GME
Happy New Year! On the heels of celebrating Martin Luther King Jr. Day at the start of the week, we encourage you to visit the UW Medicine Office of Healthcare Equity’s Cultivating a Beloved Community Mindset to Transform Unjust Systems page and participate in the UW Medicine Equity, Diversity and Inclusion Survey (more information below).
January News and Notes includes information about the Residency & Fellowship Position Appointment Agreement for 2023-2024 and our new Leave of Absence resource page for trainees. We also hope you’ll join us for upcoming events including a GME Meet & Greet for new program leadership and an Outreach event with lunch for trainees.
Also a reminder to check out Dr. Joyner’s January Blog, authored by Dr. Heather Barnett of the Care of Patients Experiencing Incarceration (CPEI) Task Force, regarding that group’s work on improving care of patients experiencing incarceration.
Please share information that you’d like included by sending to me at hamrac@uw.edu.
Thank you,
Cindy
- The GMEC has approved appointment of the following new program director; appointments await ACGME confirmation:
- Vikas O’Reilly-Shah, MD, PhD, Data and Technology in Anesthesiology
- Antonio Westphalen, MD, PhD, Abdominal Imaging (Interim)
- The GMEC approved revisions to the following policy at the December meeting. All policies are posted on the Policies and Procedures page of the GME website.
- The ACGME has a weekly e-Communication. If you wish to receive it, email ACGMECommunications@acgme.org.
Events of Interest
- Upcoming GME Lunch & Learns
- January 19: ACGME Surveys; recording and slides now available
- February 16: Workplace Safety
- March 16: Annual Program Evaluations
- GME Meet & Greet: January 2023 on January 26 from 9:00 – 9:45 am on Zoom. Join in meeting some of our GME Office staff, learning about their roles and responsibilities. This is highly recommended for new Program Directors and Program Administrators but welcome to all.
- GME Outreach Event for trainees at UWMC-ML on February 2nd from 11 am to 1 pm. We encourage trainees to stop by to say hello, meet our GME team members and take a packed lunch. Please look for an email closer to the event with specific room details.
- Please join the UW Network of Underrepresented Residents and Fellows (NURF) for a Diversity Lecture Series event by Dr. Denisse Tiznado (she/her/ella). She will be teaching about Activism Burnout & Fatigue.
- When: Monday January 30th at 7pm.
- Where: Register to receive the zoom link.
- Other GME Events can be found on our calendar.
Projects and Resources
 The GME Annual Program Timeline has been updated and is now organized by activity type, eg ACGME Accreditation, Appointments and Onboarding, Program Activities, Recruitment. Please review the updated document and note the important dates for January and February.
The GME Annual Program Timeline has been updated and is now organized by activity type, eg ACGME Accreditation, Appointments and Onboarding, Program Activities, Recruitment. Please review the updated document and note the important dates for January and February.- A new opt-in module from Learning Gateway is now available. Prioritizing Ourselves When Fatigued is a 5 minute module intended as a brief reminder on the important issue of fatigue. Programs can complete this survey to opt in for an October or January launch for trainees. Learning Gateway is happy to answer any questions about the module.
- Our new Leave of Absence webpage is now live on the GME website. Here you will find LOA planning information and resources along with an intake form to contact GME for leave planning assistance: Leave Planning Submission Form. This form can be completed by trainees or program leadership. The December 2022 Lunch & Learn on ‘Leave Policy and Guidelines’ provides an overview of both these new resources; please review the recording and slides.
- On January 17, UW Medicine launched an Equity, Diversity and Inclusion Survey to identify baseline measures of Equity, Diversity, and Inclusion across UW Medicine and provide actionable data to help prioritize areas for work at the entity and departmental levels. All UW Medicine faculty, staff, and trainees are invited to complete the survey which will take about 10-15 minutes to complete. The survey will be open until Feb. 28, 2023.
- The NRMP will be holding an Introduction to the Fellowship Match webinar for NRMP Match participating specialties on Thursday, February 16, from 10:00 – 11:00 a.m. Learn about program staff roles and responsibilities, managing your program’s participation in the Match, ranking applicants, and important policy information. Advance registration is required.
- The Huddle article “Helping Blacking Moms in Medicine Manage Child Care” features resources for our community members.
- The GME Office is currently recruiting for a Site and Contract Management Specialist, Accreditation Team (see posting, req. 212955)
People
- Alwiya Ahmed, R3, Internal Medicine, is co-author of “Trends in Labor Unionization Among US Health Care Workers, 2009-2021” in JAMA.
- Justin Bullock, fellow, Nephrology, is co-author of “Opportunities and challenges in discussing racism during primary care visits” in Health Services Research.
- The Department of Medicine was founded in 1948 with an original group of six stellar faculty members teaching and practicing at a single site. They are now the largest department at the University of Washington. Please visit their website where they look back at 75 of the changemakers who have shaped their history and 75 of their many emerging leaders who are helping to chart the path forward.
- Byron Joyner, Vice Dean for GME and DIO, is quoted in “Despite a rich history, UW struggles to enroll Black medical students” in University of Washington Magazine.
- Noam Kopmar, fellow, is lead author and Ryan Cassaday, associate professor (Hematology) is senior author of “How I Prevent and Treat Central Nervous System Disease in Adults with Acute Lymphoblastic Leukemia” in Blood.
- Henry Ou, Program Director, Pediatric Otolaryngology, is quoted in “4 reasons to put down the Q-tip and love your earwax” in Popular Science.
- Hongyang Pi, fellow, is co-lead author and Peter Leary, associate professor, and Sina Gharib, professor (Pulmonary, Critical Care and Sleep Medicine) are co-senior authors of “Metabolomic Signatures Associated With Pulmonary Arterial Hypertension Outcomes” in Circulation Research. Department of Medicine co-authors are David Ralph and Samuel Rayner.
- Andrew Portuguese, fellow, Hematology, is lead author, and Christopher Blosser, clinical professor (Nephrology) is senior author of “CD19 CAR-T therapy in solid organ transplant recipients: case report and systematic review” in Bone Marrow Transplantation. Department of Medicine co-authors are Jordan Gauthier, Scott Tykodi, Evan Hall, and Alexandre Hirayama.
- Grace Shih, Co-Director, Reproductive Health & Advocacy Fellowship, is quoted in Analysis: What the FDA’s rule changes allowing the abortion pill mifepristone to be dispensed by pharmacies mean in practice – 5 questions answered in The Conversation.
- Lindee Strizich and Chris Kim had their abstract “Fostering trainee participation in hospital patient safety event reviews,” accepted from among 1366 submissions for poster presentation in the Society of Hospital Medicine Converge Research, Innovations, and Clinical Vignette Scientific Abstract Competition.
by amande | Jan 5, 2023 | Announcements, News

Byron Joyner, MD, MPA
This month, I’ve invited Dr. Heather Barnett of the Care of Patients Experiencing Incarceration (CPEI) Task Force, partnering with GME’s Learning Gateway to share the group’s work on improving care of patients experiencing incarceration. I am very proud of this group’s work for this vulnerable population of patients we see in our hospitals.
Byron Joyner, MD, MPA
Vice Dean for GME and DIO
We are excited to share the efforts that our group has been working on to improve the care of patients in the UW Medicine System experiencing incarceration.
Background of the group
Patients incarcerated in King County’s jails are a specifically identified mission population of Harborview Medical Center, but care for this population presents unique challenges. In July 2020, the Housestaff Quality and Safety Committee (HQSC) reviewed a submission to the patient safety network in which a trainee expressed moral distress regarding the care of a patient from King County Jail who left the emergency department against medical advice despite their acute medical emergency due to the use of 4-point forensic restraints. Many residents shared similar experiences of moral distress related to limitations in care for patients experiencing incarceration. Discussions among residents led to the recognition that care for patients experiencing incarceration needed additional attention and focus. To improve care of this patient population while maintaining a safe environment for all, a group of trainees created a designated task force to further investigate current issues and targets for quality improvement.
Work so far
Survey of Healthcare workers
We conducted a survey among UW Medicine healthcare staff (including attending physicians, trainee physicians, nurses, therapists, and others) and received over 300 responses. We found that:
- Most healthcare staff did not have any specific training or education related to this patient population.

- Most healthcare staff were interested in further training to address knowledge gaps and improve patient care

- Challenges and issues providing optimal patient care were frequent.

Data Gathering
We engaged key stakeholders to determine current issues, priorities, and goals. The group gained valuable information from a variety of stakeholders.
Stakeholders
- UWMC Nurse Care Managers
- HMC ED Charge RN
- HMC ED Attending
- Correctional health physician experts, Drs. Lara Strick & Marc Stern
- King County Jail Medical Director, Dr. Benjamin Saunders
- Hospital leadership
- Harborview security
- Office of Healthcare Equity
- Physicians and activists at other institutions in San Francisco and Los Angeles
- Community members who received medical care while incarcerated
|
Education & Data Sharing
Several educational presentations and discussions were held, and preliminary resources were created:
- In May 2021, the UW HQSC-NURF Health Equity Conference was held focusing on the topic of “Caring for Patients who are Incarcerated.”
- Lara Strick and Marc Stern hosted a 3-hour training and discussion session with interested healthcare staff.
- The Task Force created preliminary training materials, including a one-pager and short video for resident and fellow use.
Additional Information
Next Steps
- To optimize educational content, we are excited to partner with GME’s eLearning team, Learning Gateway, to develop and distribute a GME-supported eLearning module for current and future residents, fellows, and (hopefully) other staff.
- This project will begin development in the Spring of 2023, with an expected 2024 launch
- We will continue to involve stakeholders, area experts, and anyone interested in supporting the project! Please get in touch!
- Possible long-term goals include evaluation of hospital policies related to care of patients experiencing incarceration and community involvement.
How to get involved

Heather Barnett, MD, PhD Acting Assistant Professor
If you are interested in being involved in the development of a training module, would like to share thoughts or feedback, or have other ways you would like to be involved, please reach out to our group by email!
by amande | Dec 21, 2022 | Announcements, Events, GME News & Notes, News
Dear GME Community,

Cindy Hamra Associate Dean, GME
As 2022 comes to an end, Happy Holidays from the GME Team to all who celebrate, and Happy New Year. This month we Reflect on the Year and we welcome our new Human Resources Manager Bre Smith (more below) to the GME team!
The December issue of GME News and Notes is brief, featuring several articles and awards, and program leadership changes. We also share information about a new Leave of Absence resource for trainees and an updated Annual Program Timeline, both designed to be resources for our community.
Please share information that you’d like to see included by sending to me at hamrac@uw.edu.
Thank you,
Cindy
Policies and Processes
- End of WA COVID-19 State of Emergency: the end of the State of Emergency indicates the end of COVID-19 paid administrative leave for workplace exposures. If a resident/fellow is sick for any reason, they can use their sick time off.
- Welcome New Program Administrators:
- Cullen McEvoy, Metabolism, Endocrinology and Nutrition
- Emma Perrow, Reproductive Endocrinology and Infertility
- The GMEC has approved appointment of the following new program directors; ACGME appointments require Review Committee (RC) confirmation:
- Faith Ross, Pediatric Cardiac Anesthesiology
- Jackie Hobbs, Psychiatry
- Thomas Soeprono, Consultation Liaison Psychiatry
- The ACGME has a weekly e-Communication. If you wish to receive it, email ACGMECommunications@acgme.org.
Events of Interest
- Upcoming GME Lunch & Learns
- December 15: Leave Policy and Guidelines; recording and slides now available
- January 19: ACGME Surveys
- February 16: Workplace Safety
- Navigating Parental Leave for Resident Physicians on January 10th from 6:30 – 7:30pm on Zoom. At this event, Hayley Fisher, GME Director of Housestaff Affairs, will educate trainees about navigating parental leave, how upcoming ACGME requirements may alter provisions and answer trainees’ questions. Register today at: https://sites.uw.edu/uwgme/event-registration/ Registration will close at 8:00am on January 9th. All residents, fellows and guests are encouraged to attend via Zoom.
- Other GME Events can be found on our calendar.
Projects and Resources
 The GME Annual Program Timeline has been updated and is now organized by activity type, eg ACGME Accreditation, Appointments and Onboarding, Program Activities, Recruitment. Please review the updated document and note the important dates for December and January.
The GME Annual Program Timeline has been updated and is now organized by activity type, eg ACGME Accreditation, Appointments and Onboarding, Program Activities, Recruitment. Please review the updated document and note the important dates for December and January.- Join us in welcoming Bre Smith, MBA, PHR, who started in the GME Office as the new HR Manager! Bre is joining UW from Seattle University where she had extensive human resources experience. In her role as the UW GME HR Manager, Bre will focus on supporting residents, fellows, and program leadership in navigating paid time off usage, leaves of absence, disability accommodations, and compliance with the CBA. We are very excited to have her join our GME team!
- Our new Leave of Absence webpage is now live on the GME website. Here you will find LOA planning information and resources along with an intake form to contact GME for leave planning assistance: Leave Planning Submission Form. This form can be completed by trainees or program leadership.
- The Annual Non-ACGME Program Survey is currently open for program directors and administrators of non-ACGME fellowship programs to complete. This survey serves to provide an annual check-in with our non-ACGME fellowship programs, identify program changes from the past year, and help identify areas where we can develop additional resources and support specific to our non-ACGME clinical fellowship programs, as defined in the GMEC-Approved (Non-ACGME Accredited) Fellowship Programs Committee (GAF) Charge and Educational Standards for Non-ACGME Programs. Responses are due by January 6.
- Early next year, the Office of Healthcare Equity will conduct a survey to better understand how personal identities, such as race, ethnicity, sex, gender, and disability, shape employee experiences at UW Medicine.
- The GME Office is currently recruiting for three roles:
- GME Float Administrator, Operations & Administration Team (see posting, req. 210821)
- RMS and Information Systems Manager, Operations and Administration Team (see posting, 213834)
- Site and Contract Management Specialist, Accreditation Team (see posting, req. 212955)
- Harborview Medical Center Emergency Alert Messages Subscription: HMC is reintroducing the UW Medicine STAT|INFO Advisory notification system to disseminate official information via text message to keep the UW Medicine workforce informed during emergencies and situations that might disrupt normal operations. Trainees are encouraged to subscribe to UW Medicine STAT|INFO ADVISORY.
- The UW Medicine Center for Scholarship in Patient Care Quality and Safety is proud to announce the (re)-launch of QI Match, an online web platform to match collaborators to quality improvement and patient safety initiatives across UW Medicine. Get started today.
People
- Justin Bullock, fellow (Nephrology) gave the 2022 American Academy of Pediatrics Plenary Session, “I’m Just Trying to Survive: A Story of Healing Through Humanity.”
- The Huddle recently featured Richard Ellenbogen, Chair of the Department of Neurological Surgery and Neurological Surgery Residency Program Director, in “Improving Neurological Surgical Education.”
- Internal Medicine Residency Program Operations Specialist, Whitney Harper, is featured in the Department of Medicine Staff Spotlight.
- Fuki Hisama, Program Director, Medical Genetics, participated in the American College of Medical Genetics and Genomics Workforce Diversity Initiative Advisory Group that assessed diversity in the medical genetics workforce. The ACMG joined major genetics and genomics organizations in releasing the Human Genetics & Genomics Workforce Survey Report. Hisama has also been named the inaugural section editor for clinical genetics for Genetics in Medicine Open, a new open access journal of the American College of Medical Genetics and Genomics, launching in January 2023.
- In 2021, the Mount Baker Foundation made a $1M pledge to the Kidney Research Institute to increase diversity in nephrology research and the workforce by supporting candidates in the early stage of their career. Christine Limonte and Justin Bullock (Nephrology) are the first UW fellows to be recipients of support from the gift.
- Michael Linenberger is profiled in Hutch News Stories. Check out “Leader in apheresis and cellular therapy, Dr. Michael Linenberger retires.”
- Linzee Mabrey, fellow, is lead author, and Mark Wurfel, professor (Pulmonary, Critical Care and Sleep Medicine) is senior author of “Plasma Interleukin-6 Predicts Clinical Decline After Completion of Dexamethasone Therapy in Severe COVID-19” in Critical Care Explorations.
- Paul Pottinger, Program Director, Infectious Diseases, is quoted in “Limits of ‘Fauci effect’: infectious disease applicants plummet, and hospitals are scrambling” in STAT.
- Paul Pottinger, Program Director, Infectious Diseases, is quoted in “Infectious diseases fellowships go unfilled for newly minted doctors” in NPR.
- Vincent Raikhel, clinical instructor, is lead author, and Chenwei Wu, clinical assistant professor (General Internal Medicine) is senior author of “Vax the Max, a Gamification Intervention for COVID-19 Vaccination Task Engagement in the Inpatient Setting” in American Journal of Medical Quality. DOM co-authors are Kevin Blau, Katherine Alberty, Paul Cornia, Rudolph Rodriguez, and Kenneth Steinberg.
by amande | Dec 8, 2022 | Announcements, News
-
 Byron Joyner, MD, MPA |
 Jennifer Best, MD |
 Cindy Hamra JD, MA |
Welcome to winter – a time of year with a heightened pace and here in the PNW, ever-present questions as to which local weather forecast will prove most accurate! Like many of you, we embrace many of these seasonal changes yet deeply feel the strain of nearly-three years, know that public health crises remain acutely active, impacting the lives and work of our community. In these (and all) moments, celebration can be a welcome antidote. Here at the end of 2022, the GME team wishes to share some of the year’s good work that we have accomplished as a community.
Over the past year, the GME Office has consistently focused on our strategic values of expertise, integration, quality and value, communication, advocacy, and people – even as we began development of a new GME strategic plan for AY2024 to 2029. Thank you to those of you who provided early input, and we look forward to sharing more information early in the new year.
Our team continues to evolve. This year, we said hello to team members Karyn Crow (GME Float Administrator), Amanda Easton (Program Manager, Operations and Administration), Jenn Johal (Learning Environment Specialist), Brandon Phanmaha (Business Analyst), Howard Schaefer (Wellness Counselor) and Bre Smith (HR Manager). Two new roles – Site and Contract Management Specialist and RMS and Information Systems Manager – have also been posted. We hope to have good news to share regarding these hires soon.
A highlight of 2022 was the successful negotiation of the Collective Bargaining Agreement between RFPU-NW and the University of Washington. During the process, GME staff actively advocated for residents and fellows to UW Medicine Leadership – and we believe that the outcome for residents and fellows represents a well-deserved step forward.
Our Sponsoring Institution received continued accreditation from the ACGME, reflecting the collective work of all of you, as well as a new ACGME Recognition status for Non-Standard Training Programs, including several of our non-ACGME accredited fellowships.
Continuing the opportunity to cultivate community and better identify and remedy needs in the learning environment, GME Leadership continued the Chief Resident/Fellow Forum. These gatherings have been increasingly attended and extremely high yield. We remain impressed by the thoughtfulness of these leaders and their creative ideas. Together, we have tackled and resolved challenges we may not otherwise have been aware of. A more recent community gathering was a convening of our growing cohort of Vice Chairs for Education – individuals filling a role supporting learners and programs across the continuum of medical education within our clinical departments We are hoping this group will work with us and with one another to develop standards, share best practices, and connect over similar work within a learning community.
The GME Office continues to partner on School of Medicine initiatives that we feel are key to the improvement of our clinical and learning environments. The first initiative is a large-scale effort to institute a program of restorative justice in response to harms within our community. Headed by Office of Healthcare Equity, this program will provide all of us with access to an alternative means of conflict resolution focused on community building. The second initiative – trainee participation in the UW Medicine Well Being Survey – is revealing actionable information on an expanded range of domains impacting trainee well-being within the workplace. We are working to compile program-level results early next year and anticipate close partnership with Dr. Anne Browning to develop action plans aligned with UW Medicine support that we hope will lesson trainee distress.
Most importantly, we want to express gratitude to each one of you. Thank you for your daily work to maximize, provide and ensure quality specialty training within UW GME with a shared goal of taking exceptional care of our patients. We welcome every opportunity to support our residents and fellows and to improve the clinical learning environment. If you have questions, concerns, or suggestions, we always want to hear from you.
Best for the holiday season and Happy New Year!
Byron Joyner, MD, MPA
Vice Dean for GME and DIO
Jennifer Best, MD
Associate Dean, Accreditation and Education
Cindy Hamra, JD
Associate Dean, Operations and Administration
by amande | Dec 1, 2023 | Announcements, Awards, News

Itay Bentov, MD
It is a pleasure to announce that Dr. Itay Bentov (Associate Professor, Department of Anesthesiology and Pain Medicine) is the winner of the 2023 Bruce C. Gilliland Award.
The Bruce C. Gilliland, M.D. Excellence in Graduate Medical Education Teaching Award was created in 2007 as a tribute to rheumatologist and academic leader Dr. Bruce Gilliland. Dr. Gilliland was a resident in Internal Medicine and a fellow in the Division of Rheumatology University of Washington, followed by a thriving faculty career at UW Medicine that spanned 45 years. Dr. Gilliland, who died in 2007 after a lengthy battle with cancer, will long be remembered for his dedication to the UW School of Medicine (UWSOM) as a mentor and as a physician.
The Gilliland Award is given annually to a faculty member actively engaged in clinical and didactic training or in the implementation of a graduate medical education curriculum. The winner must have demonstrated evidence of excellence over time and must have served at least 3 years within the UWSOM as a teacher of residents and/or fellows.
Dr. Bentov is a multi-year winner of the Department of Anesthesiology and Pain Medicine’s Golden Apple Teaching Award, which is voted on by trainees in the Department annually. In fact, he has won the Golden Apple Award nearly every year since 2010 and twice in 2016 – more than any other faculty since he joined the Department in 2008! Dr. Bentov is widely regarded by residents, fellows and faculty as one of, if not the best educators and clinicians in the Department. He has a strong record of mentorship and has served in multiple leadership positions, including serving on the UW Faculty Senate, the Faculty Council on University Relations and Chairing the Anesthesiology Grand Rounds Committee. He is nationally recognized for his expertise in the field of geriatric anesthesiology and has published extensively in the area, including the seminal chapter on this topic in Clinical Anesthesia.
Evaluations of Dr. Bentov by residents and fellows extol his comfort teaching at any level, his eagerness to share and to seamlessly tailor discussions to learners’ abilities and to patients’ needs. For example:
Dr. Bentov embodies all the qualities patients would want in a physician. He is an advocate for the residents. He is a role model and thought of in the highest regard by all residents. He challenges you to be a better physician. He is very professional to both his colleagues and staff. His passion for medicine and anesthesia is contagious. He is a mentor I will strive to emulate as my career evolves, and I think I can speak on behalf of many other residents that they too feel the same way.
On behalf of the GME Office, congratulations to Dr. Itay Bentov!

Byron Joyner, MD, MPA
Byron Joyner, MD, MPA
Vice Dean for Graduate Medical Education
Designated Institutional Official
by amande | Nov 18, 2022 | Announcements, Events, GME News & Notes, News
Dear GME Community,

Cindy Hamra Associate Dean, GME
November is Native American Heritage month, a time to celebrate and honor our Native and Indigenous communities. UW Medicine has a dedicated Huddle page with more information about Native American Heritage Month. November 8 was National First-Generation Day and two trainees were featured in this Huddle article sharing what being first generation means to them.
Two other opportunities to celebrate this month – Dr. Joyner’s November blog highlights UWSOM’s many ACGME award winners. Additionally, the University of Washington rose from No. 7 to No. 6 on the U.S. News & World Report’s Best Global Universities rankings. The UW maintained its No. 2 ranking among U.S. public institutions and placed in the top 10 in clinical medicine (No. 6).
Many thanks to those who shared information; please continue to do so by sending to me at hamrac@uw.edu.
Thank you,
Cindy
Policies and Processes
- The GMEC approved revisions to the following policies at the November meeting. All are posted on the Policies and Procedures page of the GME website:
- End of WA COVID-19 State of Emergency: the end of the State of Emergency indicates the end of COVID-19 paid administrative leave for workplace exposures. If a resident/fellow is sick for any reason, they can use their sick time off.
- The Staff Quarantine and Isolation Policy has been posted to reflect the following changes:
- Change in conventional status recs to require two negative Ag tests if early return to work, per new CDC guidance
- Changed surveillance testing- Following a higher-risk exposure, HCP should have a series of three viral tests for SARS-CoV-2 infection, day 1, 3, and 5
- Added in option for Ag testing x 2 for symptomatic employees in the FAQ
- For exposed HCP, no longer requiring a PCR in the serial testing
- The second / final GMEPAC application for academic year 2023 – 2024 (AY24) is now open. Programs that want to make changes in rotations or expansions that result in an increase in training time at any site for academic year 2023-2024 must go through the GMEPAC process (excludes VA FTE requests). Information is posted to the GME website under Committees; select “GME Position Allocation Committee (GMEPAC).” AY24 applications are due December 2, 2022.
- RFPU-NW members are entitled to one (1) paid personal holiday per calendar year. If unused in the calendar year, the personal holiday is forfeit, and it is not paid at separation. It is the employee’s responsibility to schedule the personal holiday before December 31st. See complete information in Article 12 of the RFPU-NW Contract.
- The GMEC has approved appointment of the following new program directors; ACGME appointments require Review Committee (RC) confirmation:
- Laura Romecevich, Global and Rural Health (Department of Medicine)
- Welcome New Program Administrators:
- Danielle Long, Nephrology
- Karina Martinez, Plastic Surgery
- Tiffany Wallace, Medical Genetics and Rheumatology
- The ACGME has a weekly e-Communication. If you wish to receive it, email ACGMECommunications@acgme.org.
Events of Interest
- Upcoming GME Lunch & Learns
- December 15: Leave Policy and Guidelines
- January 19: ACGME Surveys
- Residents, program directors, coordinators, and designated institutional officials are invited to hear and discuss provocative and inspiring stories of diversity, equity, inclusion, activism, and social justice from winners of the prestigious Vilcek-Gold Award for Humanism in Healthcare. The event will take place virtually, November 4. Register to Participate.
- UW Medicine has opportunities for medical and administrative volunteers for the Seattle Marathon, Nov. 26. If you are interested, please complete the 2022 Seattle Marathon Medical Team Volunteer Registration. For more information, contact rmsports@uw.edu. Residents and Fellows will need to comply with the Medical Volunteer Activities Policy (please note the 2 week advance deadline).
- Other GME Events can be found on our calendar.
Projects and Resources
 The GME Annual Program Timeline has been updated and is now organized by activity type, eg ACGME Accreditation, Appointments and Onboarding, Program Activities, Recruitment. Please review the updated document and note the important dates for November and December.
The GME Annual Program Timeline has been updated and is now organized by activity type, eg ACGME Accreditation, Appointments and Onboarding, Program Activities, Recruitment. Please review the updated document and note the important dates for November and December.- The ACGME has added an Equity Practice Toolkit to the ACGME Equity Matters online educational materials. The toolkit is available in the ACGME’s online learning portal, Access the Equity Practice Toolkit.
- Harborview Medical Center Emergency Alert Messages Subscription: HMC is reintroducing the UW Medicine STAT|INFO Advisory notification system to disseminate official information via text message to keep the UW Medicine workforce informed during emergencies and situations that might disrupt normal operations. Trainees are encouraged to subscribe to UW Medicine STAT|INFO ADVISORY.
- Please see the IT Governance: Tier 2 Clinical Education Committee presentation from Mike Leu (Professor, Fellowship Director, Head of Division of Clinical Informatics). Please contact Mike Leu with any questions or input.
- Support Black, Indigenous, People of Color (BIPOC) medical students at the UW School of Medicine. Help Healthcare Equity develop the UWSOM BIPOC Physicians Directory and add your name to the UWSOM BIPOC Physicians Directory, a directory where BIPOC students can easily talk to residents and physicians with identities similar to their own to find advice and answers to their questions.
- The UW Medicine Center for Scholarship in Patient Care Quality and Safety is proud to announce the (re)-launch of QI Match, an online web platform to match collaborators to quality improvement and patient safety initiatives across UW Medicine. Get started today.
- The GME Office is currently recruiting for three roles:
- GME Float Administrator, Operations & Administration Team (see posting, req. 210821)
- RMS and Information Systems Manager, Operations and Administration Team (see posting, 213834)
- Site and Contract Management Specialist, Accreditation Team (see posting, req. 212955)
People
- In recognition of their substantial contributions to local healthcare quality and safety, James Araujo (Gastroenterology), Bernard Ng (Rheumatology), and Karly Williams Silva (chief resident) have been awarded the title of Practitioner Lead in Quality & Safety (PLQS) within the Hospital & Specialty Medicine service line at the VA Puget Sound Health Care System.
- Congratulations to Julie Cheng (Pediatric Urology Fellow) whose abstract “Impact of Youtube Videos and Health Literacy on Postoperative Healthcare Utilization Following Pediatric Urologic Surgery” won Best Clinical Abstract Prize at the Societies for Pediatric Urology Fall Congress.
- A study recently published in Harm Reduction Journal examined a Seattle-based organization’s efforts to introduce heroin pipes as a means to diminish harms associated with injection drug use. Thomas Fitzpatrick, (fellow, Allergy and Infectious Diseases) is the study’s lead author. Read more from UW Medicine Newsroom.
- A recent study examined how markers of inflammation and angiogenesis in patients with pulmonary arterial hypertension were related to clinical outcomes across disease subtypes. Kellen Hirsch (R3, Internal Medicine) is lead author on the paper, published in the Journal of Heart and Lung Transplant. Learn more on the DOM news site.
- The Department of Biomedical Informatics and Medical Education recently launched a new Division of Clinical Informatics; and at the same time in conjunction with the Department of Pediatrics, launched a new section of Pediatric Clinical Informatics. Michael Leu, (Program Director, Clinical Informatics) is the inaugural division head and section chief. Get to know Michael Leu.
- Study sifts potential factors of device-implant complication. Machine learning identified preoperative conditions associated with poor outcomes of left-ventricle assist device surgery. Song Li, heart failure cardiologist at the UW Medicine Heart Institute is the paper’s senior author. Lead author is Arjun Bahl (R3,Internal Medicine). Read the full story from UW Medicine Newsroom.
- Despoina Michailidou, fellow, is lead author, and Bernard Ng, associate professor (Rheumatology) is senior author of “Predictive models for thromboembolic events in giant cell arteritis: A US veterans health administration population-based study” in Frontiers in Immunology. DOM co-author is Gary Lyman.
- Andrew Portuguese (fellow, Hematology) is lead author, and Hans Joachim Deeg (professor, Medical Oncology) is senior author of “Transplantation for myeloid neoplasms with antecedent solid tumor” in Cancer. DOM co-author is Aya Albittar.
- The Fall 2022 DOS Surgery Synopsis is focused on education and has lots of great features!
- Chenwei Wu, (clinical assistant professor, General Internal Medicine) was awarded the 2022 Gene Peterson Award on behalf of the UW Housestaff Quality and Safety Committee (HQSC). The award is named after Dr. Gene Peterson, who had a great appreciation for the involvement of trainees in the fields of quality improvement and patient safety, and for the unique perspective they bring to the UW.



 Please review the GME Annual Program Timeline for important dates for the months of February and March.
Please review the GME Annual Program Timeline for important dates for the months of February and March.

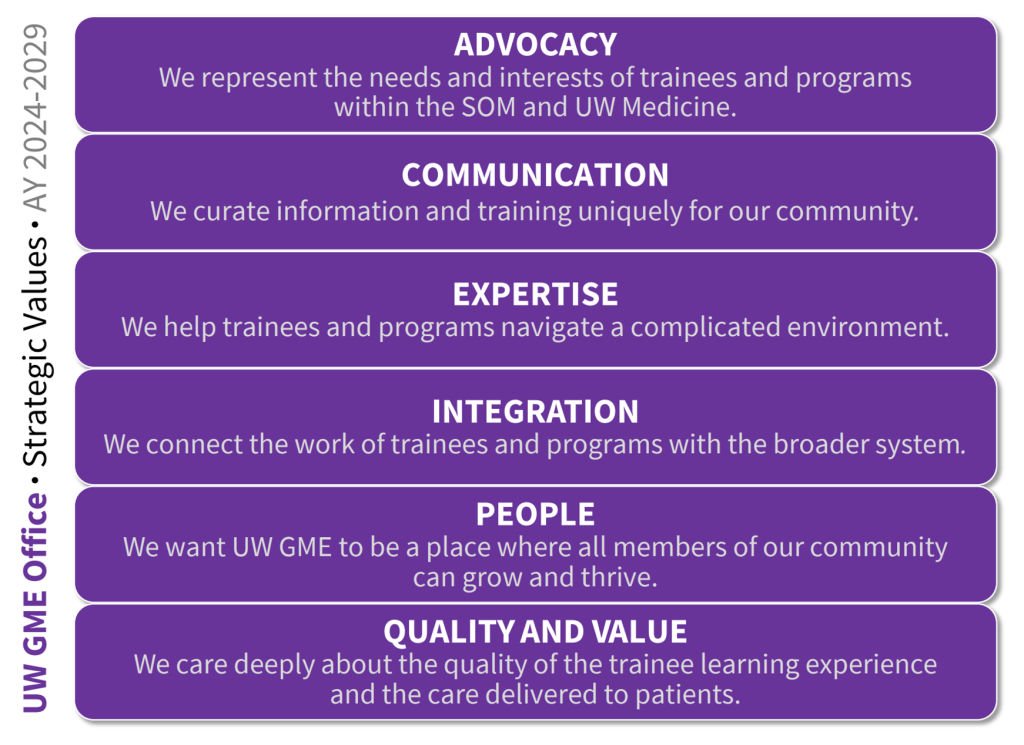

![Example of Names & Pronunciation Initiative Badge. Learn more about the project online [QR Code]. My name is pronounced:](https://sites.uw.edu/uwgme/files/2024/01/Badge-Example-25ed619a14af647a-150x150.jpeg) Implementing NPI required perseverance and teamwork to translate awareness into action. Despite facing initial setbacks in grant applications, the project eventually secured support through the 2023 UW Resilience & Compassion Seed Grant. The setting was ripe for collaboration, as I came to learn that other students, residents, fellows, attendings, and staff had also had similar conversations about the importance of correct name pronunciations. Coming together, we designed the tags, developed strategies for their distribution across the Washington, Wyoming, Alaska, Montana, Idaho (WWAMI) region, and engaged with various UW Medicine affiliated groups to foster the project’s success in our community. I also built
Implementing NPI required perseverance and teamwork to translate awareness into action. Despite facing initial setbacks in grant applications, the project eventually secured support through the 2023 UW Resilience & Compassion Seed Grant. The setting was ripe for collaboration, as I came to learn that other students, residents, fellows, attendings, and staff had also had similar conversations about the importance of correct name pronunciations. Coming together, we designed the tags, developed strategies for their distribution across the Washington, Wyoming, Alaska, Montana, Idaho (WWAMI) region, and engaged with various UW Medicine affiliated groups to foster the project’s success in our community. I also built 







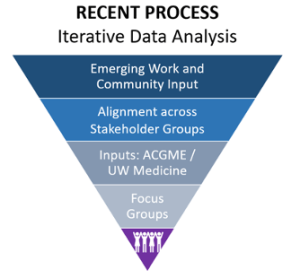
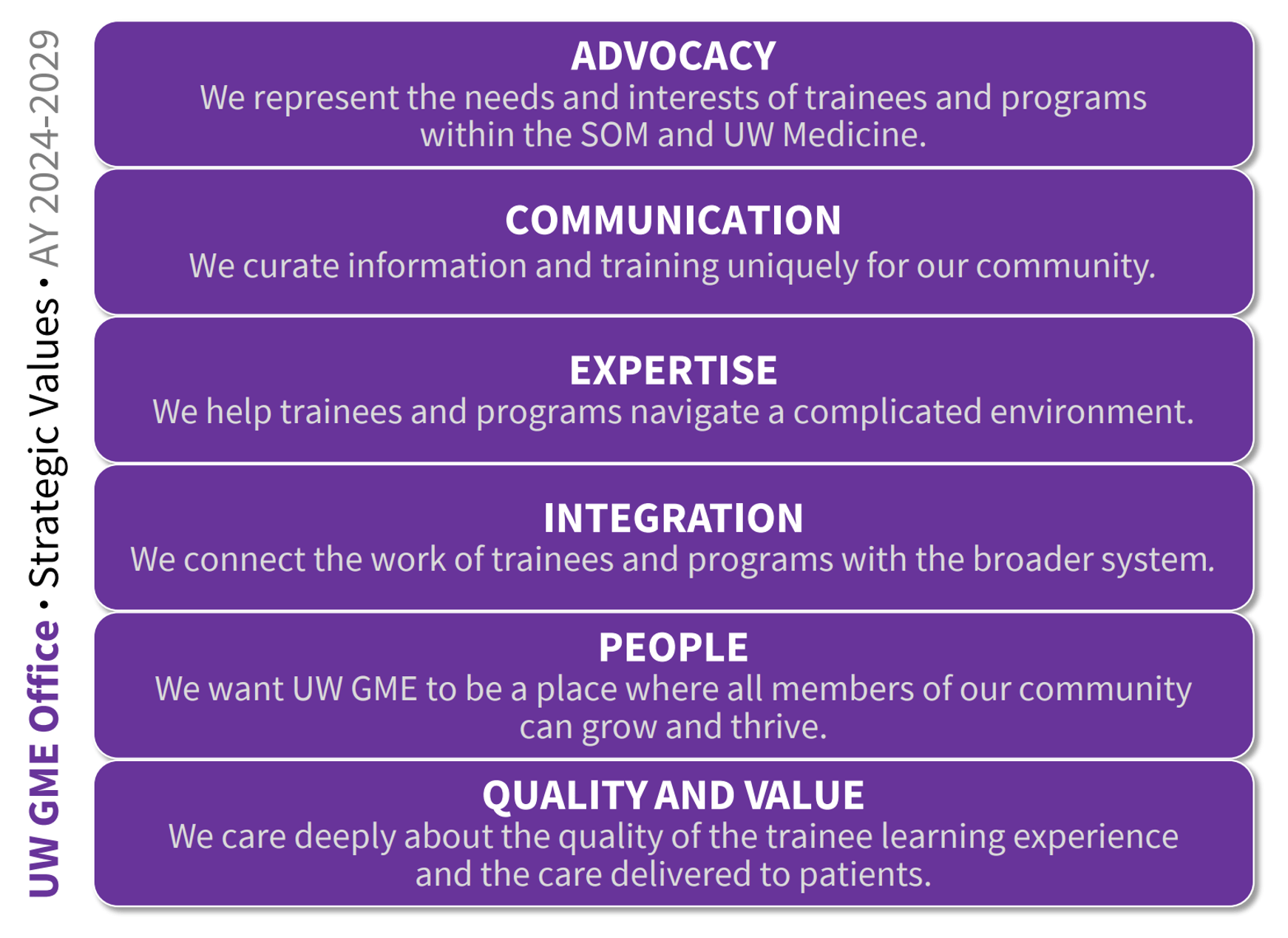
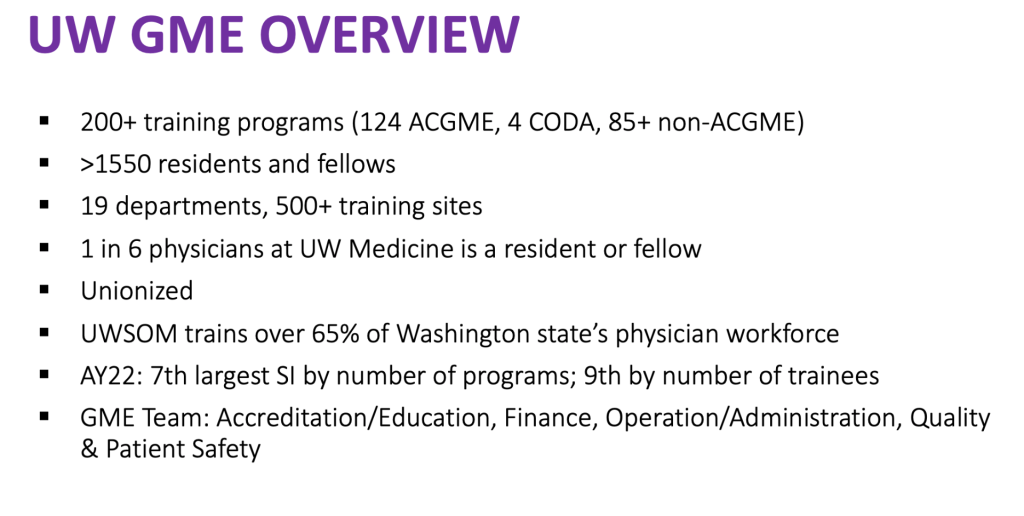
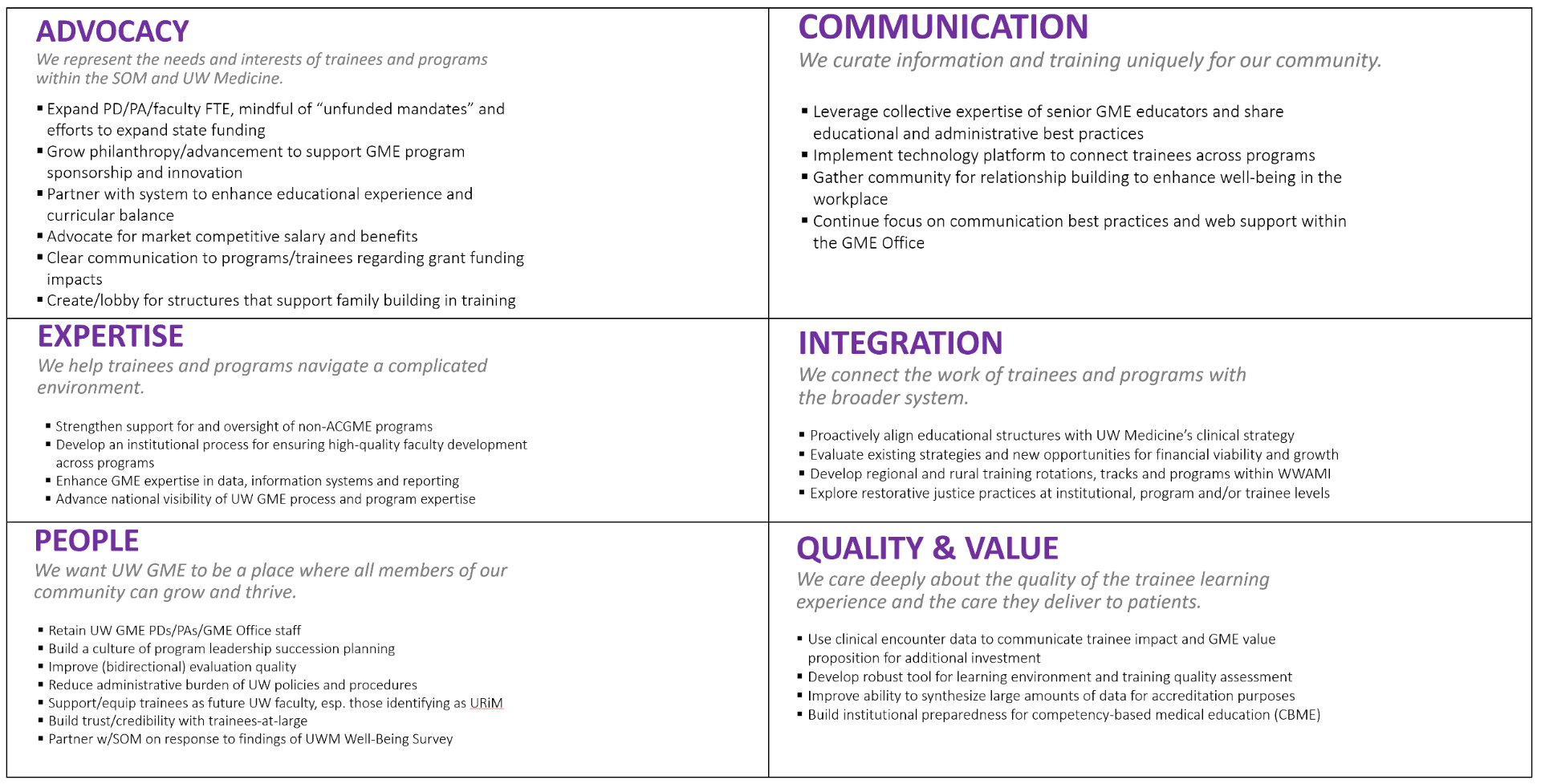
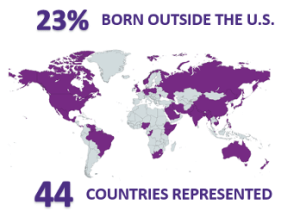

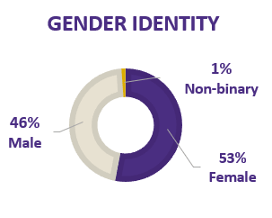

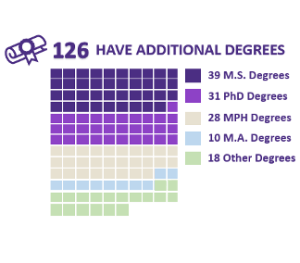
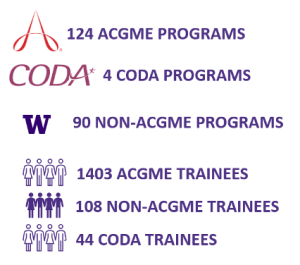
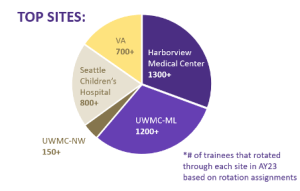
 As the new academic year begins, 502 new residents and fellows are joining UW Graduate Medical Education (GME) programs to further their medical and dental training.
As the new academic year begins, 502 new residents and fellows are joining UW Graduate Medical Education (GME) programs to further their medical and dental training.